Cervical cancer: Difference between revisions
imported>Stephen Ewen (Image:Cervical cancer.jpg) |
imported>Robert Badgett |
||
| Line 2: | Line 2: | ||
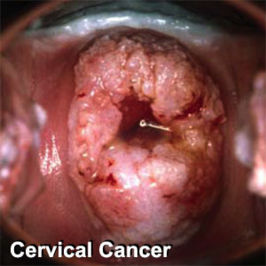
[[Image:Cervical cancer.jpg|right|thumb|266px|{{#ifexist:Template:Cervical cancer.jpg/credit|{{Cervical cancer.jpg/credit}}<br/>|}}]] | [[Image:Cervical cancer.jpg|right|thumb|266px|{{#ifexist:Template:Cervical cancer.jpg/credit|{{Cervical cancer.jpg/credit}}<br/>|}}]] | ||
==Screening== | ==Screening== | ||
===Clinical practice guidelines=== | |||
Clinical practice guidelines address [[mass screening]] for cervical cancer.<ref>(2009) [http://journals.lww.com/greenjournal/documents/PB109_Cervical_Cytology_Screening.pdf Cervical Cytology Screening]. The American College of Obstetricians and Gynecology</ref>. A summary of these guidelines is:<ref>Davis AJ. (2009) [http://womens-health.jwatch.org/cgi/content/full/2009/1123/1 Major Changes in ACOG Cervical Cytology Screening Recommendations]. Journal Watch Women's Health</ref> | |||
* "Cervical cancer screening should begin at age 21 regardless of age at onset of sexual activity." | |||
* "Cervical cytology screening from age 21 to 29 is recommended every 2 years but should be more frequent in women who are HIV-positive, are immunosuppressed, were exposed in utero to [[diethylstilbestrol]], or have been treated for [[cervical intraepithelial neoplasia]] (CIN) 2, 3 or cervical cancer." | |||
* "Women age 30 who have three consecutive negative screens and who do not fit the above criteria for more-frequent screening may be tested every 3 years. Co-testing with cervical cytology and high-risk HPV typing is also appropriate; if both tests are negative, rescreening in 3 years is warranted." | |||
* "Cervical cancer screening is unnecessary in women who have undergone hysterectomies for benign disease and who have no histories of CIN." | |||
* "Discontinuation of screening after age 65 or 70 is reasonable in women with 3 negative consecutive tests and no cervical abnormalities during the previous decade." | |||
* "Women with histories of CIN 2, 3 or cancer should undergo annual screening for 20 years after treatment." | |||
* "[[Human papilloma virus (HPV)|HPV]] vaccination does not change these recommendations." | |||
===Accuracy of screening tests=== | ===Accuracy of screening tests=== | ||
Revision as of 09:42, 1 December 2009
Screening
Clinical practice guidelines
Clinical practice guidelines address mass screening for cervical cancer.[1]. A summary of these guidelines is:[2]
- "Cervical cancer screening should begin at age 21 regardless of age at onset of sexual activity."
- "Cervical cytology screening from age 21 to 29 is recommended every 2 years but should be more frequent in women who are HIV-positive, are immunosuppressed, were exposed in utero to diethylstilbestrol, or have been treated for cervical intraepithelial neoplasia (CIN) 2, 3 or cervical cancer."
- "Women age 30 who have three consecutive negative screens and who do not fit the above criteria for more-frequent screening may be tested every 3 years. Co-testing with cervical cytology and high-risk HPV typing is also appropriate; if both tests are negative, rescreening in 3 years is warranted."
- "Cervical cancer screening is unnecessary in women who have undergone hysterectomies for benign disease and who have no histories of CIN."
- "Discontinuation of screening after age 65 or 70 is reasonable in women with 3 negative consecutive tests and no cervical abnormalities during the previous decade."
- "Women with histories of CIN 2, 3 or cancer should undergo annual screening for 20 years after treatment."
- "HPV vaccination does not change these recommendations."
Accuracy of screening tests
Papanicolaou smear
A systematic review of available studies for detection of cervical intraepithelial neoplasia grade 2 or worse found the follow results.[3]
| ASCUS or worse | High grade or worse | |||
|---|---|---|---|---|
| sensitivity | specificity | sensitivity | specificity | |
| Conventional method | 88% | 71% | 55% | 97% |
| Liquid-based thin prep | 88% | 71% | 57% | 97% |
A more recent study of the conventional method for cervical intraepithelial neoplasia of grade 2 or 3 reported very similar results:[4]
- sensitivity 55%
- specificity 94%
Human papillomavirus testing
- sensitivity 95%[4]
- specificity 97%[4]
Combined testing
If either the Papanicolaou smear or Human papillomavirus testing are abnormal:
- sensitivity 100%[4]
- specificity 93%[4]
Effectiveness of screening
In a randomized controlled trial, the addition of Human papillomavirus testing to screening for cervical cancer "reduces the incidence of grade 2 or 3 cervical intraepithelial neoplasia or cancer detected by subsequent screening examinations."[5]
In another randomized controlled trial, the addition of Human papillomavirus testing to screening for cervical cancer led to earlier detection of CIN3+ lesions.[6]
References
- ↑ (2009) Cervical Cytology Screening. The American College of Obstetricians and Gynecology
- ↑ Davis AJ. (2009) Major Changes in ACOG Cervical Cytology Screening Recommendations. Journal Watch Women's Health
- ↑ 3.0 3.1 Arbyn M, Bergeron C, Klinkhamer P, Martin-Hirsch P, Siebers AG, Bulten J (2008). "Liquid Compared With Conventional Cervical Cytology: A Systematic Review and Meta-analysis". Obstet Gynecol 111 (1): 167–177. DOI:10.1097/01.AOG.0000296488.85807.b3. PMID 18165406. Research Blogging.
- ↑ 4.0 4.1 4.2 4.3 4.4 Mayrand MH, Duarte-Franco E, Rodrigues I, et al (2007). "Human papillomavirus DNA versus Papanicolaou screening tests for cervical cancer". N. Engl. J. Med. 357 (16): 1579–88. DOI:10.1056/NEJMoa071430. PMID 17942871. Research Blogging.
- ↑ Naucler P, Ryd W, Törnberg S, et al (2007). "Human papillomavirus and Papanicolaou tests to screen for cervical cancer". N. Engl. J. Med. 357 (16): 1589–97. DOI:10.1056/NEJMoa073204. PMID 17942872. Research Blogging.
- ↑ Bulkmans NW, Berkhof J, Rozendaal L, et al (2007). "Human papillomavirus DNA testing for the detection of cervical intraepithelial neoplasia grade 3 and cancer: 5-year follow-up of a randomised controlled implementation trial". Lancet 370 (9601): 1764–72. DOI:10.1016/S0140-6736(07)61450-0. PMID 17919718. Research Blogging.