Talk:Archive:Healing Arts Workgroup: Difference between revisions
imported>Howard C. Berkowitz |
imported>John Stephenson m (moved CZ Talk:Healing Arts Workgroup to Talk:Archive:Healing Arts Workgroup: Workgroup abolished; old pages in CZ namespace may be moved to Archive namespace accorcing to http://ec.citizendium.org/wiki/EC:R-2011-011) |
||
| (13 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
{{TOC|right}} | |||
==A taxonomic strawman; let us hope it does not become a Wicker Man== | |||
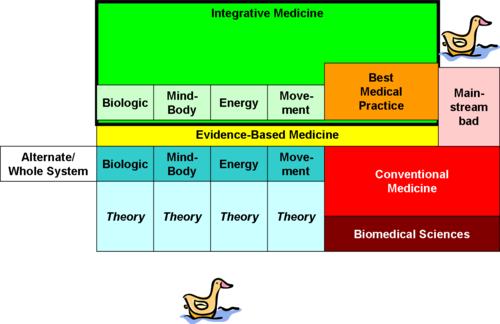
Maybe a picture will help. On the right, you have (red) [[medicine]], with a theoretical underpinning of biomedical sciences. Some of conventional medicine makes it through the filter of [[evidence-based medicine]], and combines into orange: the best common practice of standalone conventional medicine. Some of conventional medicine doesn't have supporting evidence and as much quackery as the wildest alt theory. | Maybe a picture will help. On the right, you have (red) [[medicine]], with a theoretical underpinning of biomedical sciences. Some of conventional medicine makes it through the filter of [[evidence-based medicine]], and combines into orange: the best common practice of standalone conventional medicine. Some of conventional medicine doesn't have supporting evidence and as much quackery as the wildest alt theory. | ||
[[Image:WannaBuyADuck.png|center|500px|relationships]] | [[Image:WannaBuyADuck.png|center|500px|relationships]] | ||
| Line 34: | Line 35: | ||
::::::By the way, I still think these should be contained in one article [[Complementary and Alternative medicine]] and I actually look forward to linking to an article on the the early history of the [[philosophy of medicine]] because it is also the history of the philosophy of alternative medicine as well. [[User:D. Matt Innis|D. Matt Innis]] 03:43, 30 December 2008 (UTC) | ::::::By the way, I still think these should be contained in one article [[Complementary and Alternative medicine]] and I actually look forward to linking to an article on the the early history of the [[philosophy of medicine]] because it is also the history of the philosophy of alternative medicine as well. [[User:D. Matt Innis|D. Matt Innis]] 03:43, 30 December 2008 (UTC) | ||
===Questioning the EBM paradign=== | |||
The diagram is very insightful, albeit with the usual caveat that what is considered alternative or conventional depends on culture (and therefore on time, location, religion etc.) It is, however, missing a dimension, IMHO. In addition to evidence-based medicine - a rather new concept, btw - there is much to learn from experience-based medicine as well, both from practicioner experience and from patient experience. Surveys, for instance, can generate information that is just as valuable as information from trials, and so can narrative case descriptions. Both types of knowledge, evidence-based and experience-based, feed best medical practice. [[User:Guido den Broeder|Guido den Broeder]] 16:10, 5 January 2009 (UTC) | |||
:You seem to be suggesting that EBM is exclusively about [[randomized controlled trial]]s. It is not. Historical and population date is a major part of medical knowledge. The Framingham Heart Study or the Nurses' Health Study are extremely well established observational systems, not trials. | |||
:In the U.S., adverse event reporting under FDA Phase IV is based on experience, not trials. Every week's issue of the ''New England Journal of Medicine'' contains a clinicopathologic conference about a specific case. | |||
:There are many statistical tools used in collecting evidence, which have nothing to do with trials. The U.K. Parliament characterized some at [http://www.parliament.the-stationery-office.co.uk/pa/ld199900/ldselect/ldsctech/123/12315.htm]. Very little infectious disease epidemiology is trial based, and good field investigators routinely use traditional knowledge. One well-known case is in the collaborative success of Navajo tribal healers and CDC Epidemiological Intelligence Service in the 1993 outbreak of hantavirus pulmonary syndrome; I don't have an immediate online reference, but Laurie Garrett's book, ''The Coming Plagues'', is excellent on field epidemiology. I subscribe to the ProMED mailing list, which has jokingly been called the CNN of epidemiology; it overlaps with the journal and RSS feed of ''Emerging Infectious Disease''. | |||
:Trials and hammers are good for some tasks, population statistics and screwdrives for others, and case reports and wrenches for yet other problems. I'm rather concerned about the continuing problem that EBM is necessarily RCT based. It is not. [[User:Howard C. Berkowitz|Howard C. Berkowitz]] 16:25, 5 January 2009 (UTC) | |||
:Experience is part of evidence based medicine, not separate from it. | |||
::I hear you. In fact, I argued the same when I first heard the term, only to find that everybody disagreed with me, and specifically did not consider uncontrolled settings a basis for EBM, so I had to follow their terminology. Obviously, the scientific method can be applied to any type of data. My origins are in an area of research where almost no trials exist. [[User:Guido den Broeder|Guido den Broeder]] 18:08, 5 January 2009 (UTC) | |||
:::There are several strong counterarguments that can be made. Perhaps the most important body of information on cardiovascular risk factors in the U.S. come from Framingham, Massachusetts, where it has become a tradition to cooperate with observations now, I believe for about 3 generations. Obviously, there are local factors, but it's a fairly representative community. | |||
:::Given that there are always medical politics, it's always best to argue from strength. A friend of mine decided to go to medical school later in life, and could just get into some Caribbean schools. He had been a reasonably high-level civil servant, so knew how to play games. He deliberately took his internship at a hospital in the Baltimore, MD area, where Johns Hopkins is located, and spent all his optional time at Hopkins. Earlier, he had taken biomedical engineering there. So, when he wanted an unusual residency, he had the contacts there to get in, and then develop a specialized program in public health. The accrediting authorities said, essentially, "that's weird...but it's from Hopkins, so it must be all right." | |||
:::So, when I look at integrative medicine, I look at the programs in first-rate institutions such as Hopkins, the Mayo Clinic, Harvard, Duke, etc., and point out that they operate by EBM, but don't always require trials. Memorial Sloan-Kettering now has the first funded fellowship program in pain & palliative medicine, which specifically includes training in acupuncture and other modalities with varying amounts of RCT data. | |||
:::Some quite conventional areas don't lend themsleves to classic RCT: infectious disease epidemiology, emergency medicine, and above all, surgery. Pharmacogenomics is unquestionably mainstream, but the very nature of the concept is that it will be individualized, so alternative statistical methods are being used. | |||
:::So, while it may not be fair to some complementary practitioners who have been trying for acceptance, the impetus is likely to come from the medical programs that are reaching out. There's a surprising amount of ideas, partially based on cost-effectiveness, coming from "mainstream" disciplines such as nursing and clinical pharmacy, especially in chronic disease case management. My insurer, certainly not seeing itself as casual about cost, offered me nurse case management, but, after I talked with the nurse, they were quite satisfied I could handle my own management. Lots of people can't, however, and hard financial numbers say that "mid-level" practitioners are cost-effective. I'll have to find the journals, but some nursing researchers have been innovating. For example, there's at least one trial where complete blinding was impractical, which suggests that while pure aromatherapy may smell nice but not do much, using the essential oils in conjunction with massage did have benefits. [[User:Howard C. Berkowitz|Howard C. Berkowitz]] 19:23, 5 January 2009 (UTC) | |||
::::I agree that the terms [[Evidence based medicine]] and [[Best medical practice]] are misused interchangeably and I think that we should make sure that each of those articles should make that distinction as clear as the literature will allow us. When I saw on the chart that Howard had included Best medical practice, I assumed that it represented evidence base (which includes some elements of the doctors experience) and best medical practice (which places more emphasis on this experience). At lest this is my interpretation, but there are others here that can explain it better than I. [[User:D. Matt Innis|D. Matt Innis]] 19:31, 5 January 2009 (UTC) | |||
:::::Yes, that is the way I was using best medical practice; it was a superset of trials. Let me give an example: the textbook ''Top Knife''[http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1409880], a deliberate takeoff on ''Top Gun'', by Asher Hirshberg and Ken Mattox. Mattox is arguably the dean of trauma surgery; while I've never met him in person, I have had a good deal of mailing list interaction. ''Top Knife'' is a small but fascinating book that is, essentially, nothing but experience-based information, beautifully written. It's not immediately at hand to quote, but it makes the very careful point that its total scope is in the OR with a patient open, no consultants, and you, the surgeon, are in trouble. Just as one example of the sort of thing that will never get into trials, they describe what to do with repairing an especially fragile spleen, soft enough that surgical knots pull through the tissue. They explain how to put a piece of absorbable surgical fabric on the surface, to give a place to hold the knot. How is that sort of information going to come out of an RCT? The book is full of "how did I get out of this particular surgical catastrophe that you might see three times in your career."[[User:Howard C. Berkowitz|Howard C. Berkowitz]] 19:52, 5 January 2009 (UTC) | |||
== Integrative vs. the others == | == Integrative vs. the others == | ||
| Line 97: | Line 125: | ||
::One of the things that bothers me is that mainstream medicine is, absolutely, a moving target. Homeopathy presents itself largely in a 19th century way and starts refighting 19th century battles. It was only recently that I found out new provings re being done; it wasn't easy to discover. A mainstream oriented person is apt to be more responsive to a alt practitioner who has a field that often looks at itself. How often do alt folks say "we have a new technique, or this old one isn't used any more"? That's said constantly in mainstream. It seemed like the more that I'd ask questions about modern homeopathy, the more I'd hear about things 50-200 years old. The alt med practitioners also aren't always citing mainstream work that does tend to validate them. There's also the alt vs. comp; there's much better commuications, I think, when the question is "how do we do this together?" [[User:Howard C. Berkowitz|Howard C. Berkowitz]] 17:41, 30 December 2008 (UTC) | ::One of the things that bothers me is that mainstream medicine is, absolutely, a moving target. Homeopathy presents itself largely in a 19th century way and starts refighting 19th century battles. It was only recently that I found out new provings re being done; it wasn't easy to discover. A mainstream oriented person is apt to be more responsive to a alt practitioner who has a field that often looks at itself. How often do alt folks say "we have a new technique, or this old one isn't used any more"? That's said constantly in mainstream. It seemed like the more that I'd ask questions about modern homeopathy, the more I'd hear about things 50-200 years old. The alt med practitioners also aren't always citing mainstream work that does tend to validate them. There's also the alt vs. comp; there's much better commuications, I think, when the question is "how do we do this together?" [[User:Howard C. Berkowitz|Howard C. Berkowitz]] 17:41, 30 December 2008 (UTC) | ||
== Evidence-Based Medicine and CAM disciplines == | |||
Matt gave me a link to a chiropractic professional information site, DCConsult.com. One of the first things I read is "Assessing the Quality of the Evidence Before Assessing Individual Studies of Spinal Orthopedic Tests" by Charles Herring [http://www.dcconsult.com/DisplayArticle.html?Article_ID=81]. Since one of the defining characteristics of [[integrative medicine]] is whether a technique meets at least some tests of [[evidence-based medicine]], I was glad to see this. The approach is based on the "Strength-of-Recommendation Taxonomy (SORT) method to assessing the literature1. The decision to use this method was made because it is a more patient-centered approach to grading evidence. According to the article describing the development of this method, the editors of the U.S. family medicine and primary care journals, (which includes American Family Physician, Family Medicine, The Journal of Family Practice, Journal of the American Board of Family Practice, and The British Medical Journal-USA), and the Family Practice Inquiries Network (FPIN) jointly developed this taxonomy." There is also mention of the STARD technique used by Cochrane, and another trial assessment method, QUADAS | |||
One of the first questions is whether other CAM disciplines use this method. | |||
Some general questions, presumably for Matt: How well does chiropractic fit the [[randomized controlled trial]] model? Is there an individualization issue as with [[homeopathy]]? Is it possible to do a "sham adjustment" and thus have the equivalent of a placebo, or would a typical trial be a new method (not limited to adjustment) compared to a generally accepted standard? [[User:Howard C. Berkowitz|Howard C. Berkowitz]] 20:57, 30 December 2008 (UTC) | |||
==Overgeneralizations about CAM== | |||
There's a professor at the University of Washington, James Whorton, who claims a unitary theory for CAM, [http://www.pbs.org/wgbh/pages/frontline/shows/altmed/clash/philosophy.html]but he's being selective in his discussions, focusing primarily on Western 19th century techniques, and also making an assumption that modern medicine is totally based on "allopathy", or the principles of opposites. | |||
The "allopathy" term, or that medicine is based on opposition, and it's exclusively the (wrong) approach of Western medicine, is neither correct as a universal description of modern techniques, nor does is it accurate in that traditional methods do not have concepts of opposites. | |||
Traditional Chinese medicine deals with both energy fields in meridians, but also specifically including the concept of drugs as attackers. Hsu Ta-ch'un wrote, in the eighteenth century, | |||
<blockquote>"Soldiers were introduced to eliminate violence, and, if there was no alternative, military operations must be started. Similarly, drugs were introduced to eliminate disease, and, if there is no other way, they must be employed. The principle is the same. ...it is if one were confronted by a hostile country. One takes advantage of the unilaterally marked nature of herbs and trees to attack the unilaterally dominant depots and palaces...if one checks the [enemy] at multiple places, there will be no grief over loss of life or a destroyed body.<ref name=AMN-MCI55>{{citation | |||
| title = Asian Medical Knowledge | |||
| author = Charles M. Leslie, Allan Young, American Anthropological Association | |||
| publisher = University of California Press |year = 1992 | |||
| ISBN=0520073185 | |||
| url = http://books.google.com/books?id=yCusL4oT3OoC&pg=PA55&lpg=PA55&dq=%22Hsu+Ta-ch%27un%22+Soldier&source=bl&ots=xS3ig_kTtC&sig=XkPads6jwR5XmRLKMQNaRbNy9fg&hl=en&sa=X&oi=book_result&resnum=6&ct=result#PPA56,M1}},Leslie, pp. 55-57</ref></blockquote> | |||
This is a clear example of using opposites, in [[traditional Chinese medicine]]. | |||
All conventional medicine is not based on opposites; many techniques support natural mechanisms. For example, atrial tachycardia of the heart is often treated with synchronized cardioversion: the heart rhythm is analyzed to determine where the proper heart impulse should occur, and, precisely timed, the proper beat is reinforced with an electric current, and normal rhythm recurs. In the case of ventricular fibrillation, the heart muscles are forced to discharge all at once, but the desirable outcome is that the heart again beats in synchrony with the signals generated by the sino-atrial node. Implanted demand pacemakers, like the one in my chest, only issue a signal to the heart when the expected signal from the heart is not generated. | |||
Simplifying, active immunization teaches lymphocytes to recognize a pathogen and trigger natural immune response before the invaders can reproduce. In type I diabetes, synthetic human insulins, or molecular variants, replace the insulin that the destroyed islet cells of the pancreas no longer produce. Acid-base disturbances are treated by supporting the buffering systems of the body. | |||
So, Whorton is picking selective examples to support his assertion that does apply to many, but not all, 19th century Western concepts. Traditional Chinese medicine both supports ''qi'', but also recognizes invaders. Shamanic spitting healing rituals, in multiple cultures on multiple continents, are based on removing a harmful invader that the patient cannot expel on his own. This is from Michael Harner's ''The Way of the Shaman''; I'll have page reference as soon as I find where I carefully put the book so it wouldn't be misplaced. [[User:Howard C. Berkowitz|Howard C. Berkowitz]] 03:02, 31 December 2008 (UTC) | |||
== Lessons from Homeopathy and perhaps spinoffs == | |||
Getting the homeopathy article to approval, fully understanding that approval is a milestone rather than an endpoint, I would hope the community learned some lessons from it, and perhaps from spinoff topics. There are current forum threads dealing, for example, with behavior after the Citizendium process has acted in terms of judgment and appeals. There have been questionable assertions of both discipline and individual authority over articles -- which is not to say that there are no systematic ways of defining scope for article development. | |||
There is a delicate question of whether a main article's development reflects proper development of its focus, versus when truly related subjects belong in other, links and discussions. One way of suggesting an initial scope, already used by some authors, is to start a Related Articles page even before starting the main article; while I suspect we will need additional headings in Related Articles, it is not completely unreasonable to suggest that Parent Topics suggest the required background, and subtopics, at first, may address the contents. Do remember that it is possible to associate a Definition and Related Articles with a redirect to a subheading, so putting in Subtopics that may eventually be subheadings and not articles breaks nothing. | |||
More specifically, several of us, I believe, agree that there need to be some planning metadiscussions about broad health topics that may not fit cleanly into Healing Arts, Health Sciences, and indeed Biology; there are other aspects that may be closer to History, Anthropology, Psychology, Politics, and Philosophy. I do not see, in our model of collaboration rather than confrontation, that starting consciously provocative articles is necessarily productive, unless there is some substantial consensus that this is a useful effort. I hope that [[allopathy]] does not become the Gleiwitz of another battleground; yes, Gleiwitz is an example that is very minor on its own. | |||
Where should such discussions exist? If they are in a Forum, I would urge generous storage of Forum thread URLs at various Workgroup discussion (or other) pages, as well as CZ/CZ Talk pages; while I accept that decisions were made about use of Forums as discussion, I hope that can be reexamined, especially stronger navigation tools evolve in the article space (not necessarily mainspace). | |||
I shall put some comments, only minimally modified, both in the Healing Arts forum and the Governance/Article Policy forum , fully understanding that the topics are broader than that discipline alone. I urge reflection on how to be most productive with interdisciplinary topics, topics on which different disciplines have opposing views, and disciplines that really do not define the scope of an article. | |||
I do suggest finding one primary discussion area.[[User:Howard C. Berkowitz|Howard C. Berkowitz]] 15:10, 5 January 2009 (UTC) | |||
Latest revision as of 01:04, 25 February 2012
A taxonomic strawman; let us hope it does not become a Wicker Man
Maybe a picture will help. On the right, you have (red) medicine, with a theoretical underpinning of biomedical sciences. Some of conventional medicine makes it through the filter of evidence-based medicine, and combines into orange: the best common practice of standalone conventional medicine. Some of conventional medicine doesn't have supporting evidence and as much quackery as the wildest alt theory.
Now, to the left, you have five boxes, not the neatest grouping but based on the NCCAM taxonomy. Alternative or whole systems, by definition, deal with all the healthcare needs of an individual and don't want to work with any other discipline. Perhaps the least controversial example would be a form of spiritual therapy that wants absolutely nothing but prayer, or sacrificing goats, or whatever. By its very definition, alternative medicine is alternative to everything else, and isn't going to be complementary or integrative.
To the right, there are four boxes of categories of technique. Now, there's no good way to draw something I'll explain: a given technique may be used in alternate medicine, or it might be used in complementary medicine. Complementary means "willing to play nicely with other disciplines".
Some blue complementary theories make it through the EBM filter and become light green. Bright green Integrative medicine is the combination of complementary and mainstream techniques, working together, which all meet varying standards for evidence-based medicine.
Each technique has verying levels of theory. Just like some conventional medicine doesn't make it through EBM and is quackery, some of the CAM techniques drop down and go quack-quack too.
My suspicion is that there's no one plausible theory article for CAM, any more than there's really common theory between the mechanical requirements of a replacement hip joint and the biochemical treatment of schizophrenia. The four types of CAM, to some extent, do have some commonality, although the assumptions of one energy technique, such as acupuncture , are very different from those of reflexology, and the specific discipline theory will be in the discipline-specific article.
There are cases where a given type of practitioner uses more than one class. For example, Traditional Chinese Medicine practioners use, among other things, herbals and acupuncture.
The team approach in integrated medicine can use all of the EBM-approved techiques. For some complementary techniques, the level of risk is so low, they don't interfere with other techniques, and are cheap enough that they don't need the same level of evidence as something more dangerous/interfering/costly. Howard C. Berkowitz 23:45, 29 December 2008 (UTC)
- Is this nice picture to help us here at talk or are you proposing some version of it for the article? If the latter, I would say emphatically NO. It's not intuitive, and, I would say, it's almost certainly Original Research.... (If it takes 500 words to explain a diagram, then it's not worth using. Hayford Peirce 01:39, 30 December 2008 (UTC)
- For Talk, specifically addressed to Larry's questions about how articles fit together. I would put it as a challenge to anyone thinks there is a meaningful single theory of alt med: where does it go, given all these other pieces are reasonably well defined? What theory, for example, would be common to reflexology, acupuncture, reiki, and therapeutic touch, beyond a generic "they all involve energy". Howard C. Berkowitz 02:00, 30 December 2008 (UTC)
- Though arguments could be made concerning the locations and sizes of the boxes, the jist of diagram is pretty close; that Howard shows a good understanding of the problem, which is halfway to the solution. Why don't we consider bringing this to the workgroup page where we can document the process and at the same time develop the plan for all the Healing Arts articles, not just this one. Then maybe this one will fall into place. D. Matt Innis 02:04, 30 December 2008 (UTC)
- Don't read anything into the size of the boxes -- some are that way just because it was a quick way to get the necessary text into the boxes without changing fonts, or to have certain color changes (i.e., blue passing through yellow becomes green, red passing through yellow becomes orange). And yes, green and orange, as I think of it, should have been brown. I'll be happy to take comments and fix it up, but that was 15 minutes of PowerPoint, not a more powerful graphics package or hand-drawn and scanned.
- Having a workgroup discussion is a great idea. Some of you may know this, but the first chapter of each monograph I've written has the same title: "what problem are you trying to solve.". Matt, have you an idea on how to start this? I have been trying to get simple definitions of the alt disciplines, many just stubs. I am fairly happy with integrative medicine, but if there's a better way, I won't lose sleep. If I lose weight, tell me more. :-)
- Matt, do you want a copy of the PowerPoint original? Howard C. Berkowitz 02:45, 30 December 2008 (UTC)
- Matt, have you an idea on how to start this? I have been trying to get simple definitions of the alt disciplines, many just stubs. I am fairly happy with integrative medicine, but if there's a better way, Well, I'm pretty sure that if we put you on the NCCAM board of directors, you could work this out fairly quickly. The problem is that the rational approach won't necessarily define the circular reality. I am convinced that governments have combined complementary and alternative approaches because they cannot be reasonably separated cleanly. We can define the terms as 'alternative' and 'complementary', but it is unlikely that we can place anything cleanly in a particular bracket. Then, I agree, we can relate the degree of alternative or complementary a practice can be in their own articles. Integrative is just the cutting edge description for those practises that consumer demand is causing conventional medicine to evaluate and incorporate into their paradigms.
- Sure, send me the Powerpoint original and if something hits me that I can improve, I'll send it back.
- D. Matt Innis 03:34, 30 December 2008 (UTC)
- By the way, I still think these should be contained in one article Complementary and Alternative medicine and I actually look forward to linking to an article on the the early history of the philosophy of medicine because it is also the history of the philosophy of alternative medicine as well. D. Matt Innis 03:43, 30 December 2008 (UTC)
Questioning the EBM paradign
The diagram is very insightful, albeit with the usual caveat that what is considered alternative or conventional depends on culture (and therefore on time, location, religion etc.) It is, however, missing a dimension, IMHO. In addition to evidence-based medicine - a rather new concept, btw - there is much to learn from experience-based medicine as well, both from practicioner experience and from patient experience. Surveys, for instance, can generate information that is just as valuable as information from trials, and so can narrative case descriptions. Both types of knowledge, evidence-based and experience-based, feed best medical practice. Guido den Broeder 16:10, 5 January 2009 (UTC)
- You seem to be suggesting that EBM is exclusively about randomized controlled trials. It is not. Historical and population date is a major part of medical knowledge. The Framingham Heart Study or the Nurses' Health Study are extremely well established observational systems, not trials.
- In the U.S., adverse event reporting under FDA Phase IV is based on experience, not trials. Every week's issue of the New England Journal of Medicine contains a clinicopathologic conference about a specific case.
- There are many statistical tools used in collecting evidence, which have nothing to do with trials. The U.K. Parliament characterized some at [1]. Very little infectious disease epidemiology is trial based, and good field investigators routinely use traditional knowledge. One well-known case is in the collaborative success of Navajo tribal healers and CDC Epidemiological Intelligence Service in the 1993 outbreak of hantavirus pulmonary syndrome; I don't have an immediate online reference, but Laurie Garrett's book, The Coming Plagues, is excellent on field epidemiology. I subscribe to the ProMED mailing list, which has jokingly been called the CNN of epidemiology; it overlaps with the journal and RSS feed of Emerging Infectious Disease.
- Trials and hammers are good for some tasks, population statistics and screwdrives for others, and case reports and wrenches for yet other problems. I'm rather concerned about the continuing problem that EBM is necessarily RCT based. It is not. Howard C. Berkowitz 16:25, 5 January 2009 (UTC)
- Experience is part of evidence based medicine, not separate from it.
- I hear you. In fact, I argued the same when I first heard the term, only to find that everybody disagreed with me, and specifically did not consider uncontrolled settings a basis for EBM, so I had to follow their terminology. Obviously, the scientific method can be applied to any type of data. My origins are in an area of research where almost no trials exist. Guido den Broeder 18:08, 5 January 2009 (UTC)
- There are several strong counterarguments that can be made. Perhaps the most important body of information on cardiovascular risk factors in the U.S. come from Framingham, Massachusetts, where it has become a tradition to cooperate with observations now, I believe for about 3 generations. Obviously, there are local factors, but it's a fairly representative community.
- Given that there are always medical politics, it's always best to argue from strength. A friend of mine decided to go to medical school later in life, and could just get into some Caribbean schools. He had been a reasonably high-level civil servant, so knew how to play games. He deliberately took his internship at a hospital in the Baltimore, MD area, where Johns Hopkins is located, and spent all his optional time at Hopkins. Earlier, he had taken biomedical engineering there. So, when he wanted an unusual residency, he had the contacts there to get in, and then develop a specialized program in public health. The accrediting authorities said, essentially, "that's weird...but it's from Hopkins, so it must be all right."
- So, when I look at integrative medicine, I look at the programs in first-rate institutions such as Hopkins, the Mayo Clinic, Harvard, Duke, etc., and point out that they operate by EBM, but don't always require trials. Memorial Sloan-Kettering now has the first funded fellowship program in pain & palliative medicine, which specifically includes training in acupuncture and other modalities with varying amounts of RCT data.
- Some quite conventional areas don't lend themsleves to classic RCT: infectious disease epidemiology, emergency medicine, and above all, surgery. Pharmacogenomics is unquestionably mainstream, but the very nature of the concept is that it will be individualized, so alternative statistical methods are being used.
- So, while it may not be fair to some complementary practitioners who have been trying for acceptance, the impetus is likely to come from the medical programs that are reaching out. There's a surprising amount of ideas, partially based on cost-effectiveness, coming from "mainstream" disciplines such as nursing and clinical pharmacy, especially in chronic disease case management. My insurer, certainly not seeing itself as casual about cost, offered me nurse case management, but, after I talked with the nurse, they were quite satisfied I could handle my own management. Lots of people can't, however, and hard financial numbers say that "mid-level" practitioners are cost-effective. I'll have to find the journals, but some nursing researchers have been innovating. For example, there's at least one trial where complete blinding was impractical, which suggests that while pure aromatherapy may smell nice but not do much, using the essential oils in conjunction with massage did have benefits. Howard C. Berkowitz 19:23, 5 January 2009 (UTC)
- I agree that the terms Evidence based medicine and Best medical practice are misused interchangeably and I think that we should make sure that each of those articles should make that distinction as clear as the literature will allow us. When I saw on the chart that Howard had included Best medical practice, I assumed that it represented evidence base (which includes some elements of the doctors experience) and best medical practice (which places more emphasis on this experience). At lest this is my interpretation, but there are others here that can explain it better than I. D. Matt Innis 19:31, 5 January 2009 (UTC)
- Yes, that is the way I was using best medical practice; it was a superset of trials. Let me give an example: the textbook Top Knife[2], a deliberate takeoff on Top Gun, by Asher Hirshberg and Ken Mattox. Mattox is arguably the dean of trauma surgery; while I've never met him in person, I have had a good deal of mailing list interaction. Top Knife is a small but fascinating book that is, essentially, nothing but experience-based information, beautifully written. It's not immediately at hand to quote, but it makes the very careful point that its total scope is in the OR with a patient open, no consultants, and you, the surgeon, are in trouble. Just as one example of the sort of thing that will never get into trials, they describe what to do with repairing an especially fragile spleen, soft enough that surgical knots pull through the tissue. They explain how to put a piece of absorbable surgical fabric on the surface, to give a place to hold the knot. How is that sort of information going to come out of an RCT? The book is full of "how did I get out of this particular surgical catastrophe that you might see three times in your career."Howard C. Berkowitz 19:52, 5 January 2009 (UTC)
Integrative vs. the others
To some extent I agree, and to some extent I disagree, with the idea that CAM can't be separated. There is a set of techniques that may or may not meet requirements of evidence-based medicine. By that, I don't necessarily mean randomized controlled trial; the British Parliamentary report is quite good on addressing other forms of evidence.
The World Health Organization is starting to use the term "traditional, complementary and alternative", which confuses things even more. I'm still chuckling over a situation where a hospital, which considered itself very flexible, was doing everything it could to make a Lakota Sioux patient feel cared-for, which included giving full respect to a tribal healer working with them. There was a genuine humility and interest on all sides. Things, unfortunately, rather hit the fan, when the hospital, which had a draconian no-smoking policy, discovered that the ritual used tobacco. Eventually, they just said "turn off the oxygen, wait a while for the bedding to equilibriate with room air, and then just close the door during the rite."
The principal difference I see in complementary and alternative is not, by and large, in the techniques. It is a willingness to work with other disciplines. For example, a spiritual healer that is willing to be involved if and only if prayer is the only modality used is alternative. I have, incidentally, fired MDs that variously were not willing to get second opinions in their specialties, or opinions in another relevant specialty, or honor my informed consent or refusal to something they wanted.
Alternative, to me, means a failing mark in "plays nicely with others". Complementary means "there are multiple ways. Let's see if we can work together." Integrative is an agreement for a real group of assorted practitioners to sit down and figure out where they can help one another, and, of course, the patient.
I guess I don't look at "consumer demand" as a factor. Howard C. Berkowitz 04:35, 30 December 2008 (UTC)
- Traditional are those practices that are indigenous to a region, i.e. herbs to the Navajo tribes, etc.. Conventional as we see it is not always traditional in every country that the WHO oversees. Because they are also a political organization, they have chosen this way to include the various beliefs that exist in undeveloped worlds as well.
- In many ways, medicine was not 'playing well with others' in not recognzing them as legit forms of therapy until the 1983 Wilks Antitrust suit in which they were no longer allowed to boycott chiropractic. So, again, it depends on your perspective as to who is playing nicely with whom. Most of these professions, including chiropractic developed educational systems independent of medicine in order to be able to continue to practice their disciplines. As new and more creative ways of researching began in the 1970s, spinal manipulation began to show promise for low back pain, but it wasn't until the 1990s when the US government came out with guidelines for the treatment of low back pain that had spinal manipulation as one of the top choices (and more significantly that surgery was overused) that medicine had a wake up call. In the late 1990s, the report surfaced that americans were spending more on alternative medicines out of pocket than payments to primary care. If one accepts that alternative medicine is placebo effect, then the motivation to integrate alternative medicine into conventional medicine must have been market driven - consumer driven rather than science based. Otherwise, you accept that the placebo effect is more than just doing nothing and it would be a legitimate practice. D. Matt Innis 05:08, 30 December 2008 (UTC)
- Matt, I don't disagree at all that medicine didn't play nice with chiropractic; I'm more used to having medical specialties fighting with each other. I remember, a couple days after heart surgery, feeling a little puckish, and, when my surgeon came on rounds, students in tow, I asked him if he was really cardiothoracic board certified. He did a doubletake until I explained "you treat everyone with respect. The nurses think more of you than any other surgeon. When you found out that I knew something about the upcoming surgery, you spent an hour and a half on the phone with me, discussing details. Your teaching is superb but you never humiliate anyone on rounds. How can you call yourself a self-respecting cardiac surgeon?"
- I know there are a lot of animosities, and justification. Nevertheless, what I hope we can do here is try to focus on how things work, and not refight the battles. There's a friend I'd like to get involved here, but I would like things to be more peaceful -- he's a DO double-boarded in family and emergency medicine, with an exceptional amount of field medicine experience. I think he's one of the best, open, healers around.
- What I'm about to say may seem weird, but bear with me. You know I've been doing a lot of work on Vietnam. One of the many mistakes was not starting to secure villages, and then spreading out from them, winning the countryside. I look at integrative medicine as something like smart pacification. You start from a point of agreement, and then start spreading out like an oil drop on water. Integrative people are looking to find ways to cooperate, not battle. I doubt it's perfect, but I think it's a much more likely way to get good work done than setting up discipline against discipline, or going into philosophical or cultural arguments.
- Sometimes the right things get done for the wrong reason. Now, spinal manipulation is not at all a field of expertise for me, but I've heard a few presentations that suggested that the alignment might be less the value than the neurotransmitter releases that it causes. One pain management specialist wondered if this sort of release might reset the nociceptive transmission paths in the spine, much as capsaicin resets the Substance P level in the peripheral nerves. One of the most ironic things in the Nobel saga for insulin is that one of the first patients saved was a young doctor named George Minot, who later got his own Nobel for the treatment of pernicious anemia -- which we now know he really didn't understand on a molecular basis but picked a treatment that did work.
- You may have noticed that I've done some work on placebo, and Gareth has some ideas for it. I am not, however, out to establish CAM is placebo effect. My biggest complaint about homeopathy is I still don't have a real sense of how diagnosis and remedy selection works. Before I look at trials, I'd like to understand the mechanism. I'm willing to suspend disbelief about innate intelligence or vital force or inhibitory neurotransmitter agonists until I understand the theory involving them. I'd like to see CAM articles starting with a good explanations of the practitioner's idea of what is done, and not immediately get into efficacy arguments.
- You could call me, I suppose, spiritual but not religious. I have spent time in ICUs, watching a patient's monitor before, during, and after spiritual rituals. There were objective changes. I don't know what caused them. They dissipated, but they could be repeated.
- Can we find a way to start out by defining the problem statements for the disciplines before we get into a fight about them? Never mind homeopaths and physicians -- you want something scary, find out that you are standing between an interventional cardiologist and a cardiac surgeon!Howard C. Berkowitz 05:47, 30 December 2008 (UTC)
- Thinking a little further, can we agree to disagree on consumer effect and focus on descriptions? I would also like to find acceptable terminology, which applies just as much to cardiology as chiropractic, for the varying levels of evidence supporting an intervention, as well as risks. When anything is numeric, I think is has to be expressed in appropriate statistical terms and comparisons -- it doesn't tell me much if I hear procedure A had 6000 deaths and B had 20, without knowing that A was used in a million patients and B in 100.Howard C. Berkowitz 07:04, 30 December 2008 (UTC)
- Can we find a way to start out by defining the problem statements for the disciplines before we get into a fight about them? Absolutely, let's not ever fight about them!
- can we agree to disagree on consumer effect and focus on descriptions Sure, this is not important to write about and would take lots of expert guidance and input. I just bring it up as a reason why the apparent "time has come" for the idea of integrating alternatives into medicine. There is scholarly work crediting women with keeping alternative methods alive during the years that medicine prohibited them from practicing medicine. Midwifery for example and the "old wives tales" of remedies, etc., but this would be in a history article I think. Interesting that you bring up Vietnam as that was when, in the US at least, respect for authority began to break down - Watergate, etc., those pesky hippie days and women's rights and all. These methods made a comeback then as well. It's not so much about being against medicine or science, it was about being self-reliant; free to make your own choices.. and finally it involved a sense of being a part of something bigger - elan vital/qi - that conected us to everything else. Ideas such as morphogenesis and life being about the 'energy' that holds us together rather than the material that we see. Anyway, sure, we don't have to talk about it :-) D. Matt Innis 16:17, 30 December 2008 (UTC)
Nostalgia
This is aside, but I have to do something about the coffee in my nose.
Unfortunately, one loses track of friends over the years. One such was an nurse-midwife, admittedly with a master's (mistress's?) degree in the subject, so it wasn't just tradition. It happened that we both are interested in neopaganism, so we could look at historical and current methods. One day, she whispered that she was going to whisper on of the secrets of her art, as to why everyone is sent to boil water at home deliveries: Midwifes love pasta The funny thing is that she's of Italian heritage, her husband's is Irish, yet he is the spectacular Italian cook.
Respect for authority is one factor, although I was questioning doctors before I reached puberty. Now, I do believe in an idea of connectedness among us, but I tend to think of that as orthogonal to the more mechanistic healing techniques. That's not very clear, so let me try it differently. I have very seriously used, and participated in, some traditional and other healing rites, but I very much regarded them as complementary and incommensurable with the more rationalistic healing models. One of the hot topics in some of the bioethics journals is what to do patients can ask clinicians to pray with them, when their beliefs are different. There are also a lot of issues of at least apparently more informed "consumers", which is an extremely complex area. Somewhat to my surprise, I sent a letter to the editor of one major bioethics journal, about a different view of informed consent: what if the patient wants more detail than an informed conformed form gives, and, in the wording of the Declaration of Helsinki, can reasonably be expected to understand it? For me, one of the challenges in some of the alt areas is that it's much harder to get detailed information than it is in mainstream.
That may be an area where we can be a resource: clear language on the processes, which is still a frustration of mine with homeopathy. I have a reasonable idea, I think, of how a TCM practioner takes a history and physical, and then makes choices about what treatments to use. I still don't really have a good idea what happens in a homeopathic office visit for a new patient. I have very good ideas what happens in a first evealuation with a lot of medical sciences.
If we can have articles that explain the principles of a discipline, that is neither evangelistic nor Quackwatch level, we might have a good start. FAQs aren't quite what I mean, but getting the basic principles and techniques down.
Integration discussions and how to improve both patient choice and clinician cooperation is something that can be approached in parallel. Howard C. Berkowitz 16:51, 30 December 2008 (UTC)
- I agree that we can do it with neither evangelistic nor Quackwatch levels of passion. Have you seen DC Consult. I can send you some of the other links as well. We have some new EBM practice guidelines coming out that I think is the sort of thing you were looking for. I also think the link that Gareth gave us made some strong connections that we can use. I tend to be interested in history as I like to understand the 'whys' as much as the 'whats' and I have some sources for that as well. Most are at least partially accessible online. D. Matt Innis 17:08, 30 December 2008 (UTC)
- By the way, I think that what tends to happen is that alt med people start to get defensive when they are hit with 'mainstream medicine says so and so is rubish'. I think mainstream medicine is a moving target as much as alternative medicine. Any ideas about how to handle that. I guess specific attribution is the most reasonable way. D. Matt Innis 17:11, 30 December 2008 (UTC)
- You are on the track of something. I both manage my own mainstream care and often act as an advocate for others. I see reasonably well-educated patients blown off by physicans when I don't have any problem conversing, seriously, with the same physician. The difference, in part, comes from 40 plus years of studying the ways that physicians talk to each other, and there is a certain way of organizing discussions that says "peer" to them.
- The integrative people start from the premise that they have something in common, and work out from there. There's more willingness to learn language of the other group.
- I see routine battles among different medical specialties that sound rather like what you are describing. Noninvasive cardiologist vs. cardiovascular surgeon vs. interventional cardiologist is always good for laughs.
- One of the things that bothers me is that mainstream medicine is, absolutely, a moving target. Homeopathy presents itself largely in a 19th century way and starts refighting 19th century battles. It was only recently that I found out new provings re being done; it wasn't easy to discover. A mainstream oriented person is apt to be more responsive to a alt practitioner who has a field that often looks at itself. How often do alt folks say "we have a new technique, or this old one isn't used any more"? That's said constantly in mainstream. It seemed like the more that I'd ask questions about modern homeopathy, the more I'd hear about things 50-200 years old. The alt med practitioners also aren't always citing mainstream work that does tend to validate them. There's also the alt vs. comp; there's much better commuications, I think, when the question is "how do we do this together?" Howard C. Berkowitz 17:41, 30 December 2008 (UTC)
Evidence-Based Medicine and CAM disciplines
Matt gave me a link to a chiropractic professional information site, DCConsult.com. One of the first things I read is "Assessing the Quality of the Evidence Before Assessing Individual Studies of Spinal Orthopedic Tests" by Charles Herring [3]. Since one of the defining characteristics of integrative medicine is whether a technique meets at least some tests of evidence-based medicine, I was glad to see this. The approach is based on the "Strength-of-Recommendation Taxonomy (SORT) method to assessing the literature1. The decision to use this method was made because it is a more patient-centered approach to grading evidence. According to the article describing the development of this method, the editors of the U.S. family medicine and primary care journals, (which includes American Family Physician, Family Medicine, The Journal of Family Practice, Journal of the American Board of Family Practice, and The British Medical Journal-USA), and the Family Practice Inquiries Network (FPIN) jointly developed this taxonomy." There is also mention of the STARD technique used by Cochrane, and another trial assessment method, QUADAS
One of the first questions is whether other CAM disciplines use this method.
Some general questions, presumably for Matt: How well does chiropractic fit the randomized controlled trial model? Is there an individualization issue as with homeopathy? Is it possible to do a "sham adjustment" and thus have the equivalent of a placebo, or would a typical trial be a new method (not limited to adjustment) compared to a generally accepted standard? Howard C. Berkowitz 20:57, 30 December 2008 (UTC)
Overgeneralizations about CAM
There's a professor at the University of Washington, James Whorton, who claims a unitary theory for CAM, [4]but he's being selective in his discussions, focusing primarily on Western 19th century techniques, and also making an assumption that modern medicine is totally based on "allopathy", or the principles of opposites.
The "allopathy" term, or that medicine is based on opposition, and it's exclusively the (wrong) approach of Western medicine, is neither correct as a universal description of modern techniques, nor does is it accurate in that traditional methods do not have concepts of opposites.
Traditional Chinese medicine deals with both energy fields in meridians, but also specifically including the concept of drugs as attackers. Hsu Ta-ch'un wrote, in the eighteenth century,
"Soldiers were introduced to eliminate violence, and, if there was no alternative, military operations must be started. Similarly, drugs were introduced to eliminate disease, and, if there is no other way, they must be employed. The principle is the same. ...it is if one were confronted by a hostile country. One takes advantage of the unilaterally marked nature of herbs and trees to attack the unilaterally dominant depots and palaces...if one checks the [enemy] at multiple places, there will be no grief over loss of life or a destroyed body.[1]
This is a clear example of using opposites, in traditional Chinese medicine.
All conventional medicine is not based on opposites; many techniques support natural mechanisms. For example, atrial tachycardia of the heart is often treated with synchronized cardioversion: the heart rhythm is analyzed to determine where the proper heart impulse should occur, and, precisely timed, the proper beat is reinforced with an electric current, and normal rhythm recurs. In the case of ventricular fibrillation, the heart muscles are forced to discharge all at once, but the desirable outcome is that the heart again beats in synchrony with the signals generated by the sino-atrial node. Implanted demand pacemakers, like the one in my chest, only issue a signal to the heart when the expected signal from the heart is not generated.
Simplifying, active immunization teaches lymphocytes to recognize a pathogen and trigger natural immune response before the invaders can reproduce. In type I diabetes, synthetic human insulins, or molecular variants, replace the insulin that the destroyed islet cells of the pancreas no longer produce. Acid-base disturbances are treated by supporting the buffering systems of the body.
So, Whorton is picking selective examples to support his assertion that does apply to many, but not all, 19th century Western concepts. Traditional Chinese medicine both supports qi, but also recognizes invaders. Shamanic spitting healing rituals, in multiple cultures on multiple continents, are based on removing a harmful invader that the patient cannot expel on his own. This is from Michael Harner's The Way of the Shaman; I'll have page reference as soon as I find where I carefully put the book so it wouldn't be misplaced. Howard C. Berkowitz 03:02, 31 December 2008 (UTC)
Lessons from Homeopathy and perhaps spinoffs
Getting the homeopathy article to approval, fully understanding that approval is a milestone rather than an endpoint, I would hope the community learned some lessons from it, and perhaps from spinoff topics. There are current forum threads dealing, for example, with behavior after the Citizendium process has acted in terms of judgment and appeals. There have been questionable assertions of both discipline and individual authority over articles -- which is not to say that there are no systematic ways of defining scope for article development.
There is a delicate question of whether a main article's development reflects proper development of its focus, versus when truly related subjects belong in other, links and discussions. One way of suggesting an initial scope, already used by some authors, is to start a Related Articles page even before starting the main article; while I suspect we will need additional headings in Related Articles, it is not completely unreasonable to suggest that Parent Topics suggest the required background, and subtopics, at first, may address the contents. Do remember that it is possible to associate a Definition and Related Articles with a redirect to a subheading, so putting in Subtopics that may eventually be subheadings and not articles breaks nothing.
More specifically, several of us, I believe, agree that there need to be some planning metadiscussions about broad health topics that may not fit cleanly into Healing Arts, Health Sciences, and indeed Biology; there are other aspects that may be closer to History, Anthropology, Psychology, Politics, and Philosophy. I do not see, in our model of collaboration rather than confrontation, that starting consciously provocative articles is necessarily productive, unless there is some substantial consensus that this is a useful effort. I hope that allopathy does not become the Gleiwitz of another battleground; yes, Gleiwitz is an example that is very minor on its own.
Where should such discussions exist? If they are in a Forum, I would urge generous storage of Forum thread URLs at various Workgroup discussion (or other) pages, as well as CZ/CZ Talk pages; while I accept that decisions were made about use of Forums as discussion, I hope that can be reexamined, especially stronger navigation tools evolve in the article space (not necessarily mainspace).
I shall put some comments, only minimally modified, both in the Healing Arts forum and the Governance/Article Policy forum , fully understanding that the topics are broader than that discipline alone. I urge reflection on how to be most productive with interdisciplinary topics, topics on which different disciplines have opposing views, and disciplines that really do not define the scope of an article.
I do suggest finding one primary discussion area.Howard C. Berkowitz 15:10, 5 January 2009 (UTC)
- ↑ Charles M. Leslie, Allan Young, American Anthropological Association (1992), Asian Medical Knowledge, University of California Press, ISBN 0520073185,Leslie, pp. 55-57