Bariatric surgery: Difference between revisions
imported>Shane McSweeney |
imported>Shane McSweeney |
||
| Line 70: | Line 70: | ||
<ref>Insert footnote text here</ref>Ashrafian, H. Le roux, C. " Metabolic surgery and gut hormones- A review of bariatric entero-humoral modulation" Physiology and behaviour. (2009) 620-631[http://www.sciencedirect.com/science?_ob=MImg&_imagekey=B6T0P-4VWB1BD-4-3&_cdi=4868&_user=10&_orig=search&_coverDate=07%2F14%2F2009&_sk=999029994&view=c&wchp=dGLzVtz-zSkzk&md5=3b8eb3b1242c0ef7fa254a9aa72f2d2b&ie=/sdarticle.pdf] | |||
<ref>Insert footnote text here</ref> Broberger, C. "Brain Regulation of food intake and appetite: molecules and networks" Journal of internal Medicine (2005); 258: 301-327.[http://www.ncbi.nlm.nih.gov/pubmed/16164570] | |||
<ref>Insert footnote text here</ref>DeMara. "Bariatric Surgery for Morbid Obesity". The new England Journal of Medicine (2007); 356; 2176-83 [http://content.nejm.org/cgi/content/short/356/21/2176] | |||
Revision as of 05:53, 18 October 2009
This page was started in the framework of an Eduzendium course and needs to be assessed for quality. If this is done, this {{EZnotice}} can be removed.
A brief overview of your interest group (be sure to put its name in bold in the first sentence) and the scope of the article goes here.[1]
The following list of sections should serve as a loose guideline for developing the body of your article. The works cited in references 2-5 are all fake; their purpose is to serve as a formatting model for your own citations.
Introduction
Surgery as a treatment for obesity
For many obese patients, diets and lifestlye changes do not work in long term. Bariatric surgery has proved to be the only effective method in the long term treatment of obesity.
How surgery works
Bariatric surgery works by altering the anatomy of the gastrointestinal tract, thus: limiting the volume of food the stomach can hold, interfering with the absorption of calories, and by interfering with orexigenic and anorexigenic signalling between the gut, adipose tissues and the brain.
Bariatric Surgical Procedures
Restrictive Surgery
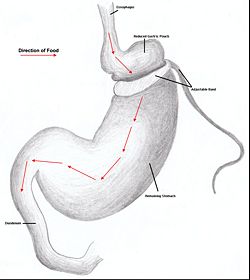
Restrictive surgery reduces the size of the stomach causing decreased hunger and an increased satiety following ingestion of smaller amounts of food. Surgical procedures include gastric banding, where an adjustable band is clipped just below the cardia of the stomach creating a small gastric pouch above(kerrigan, le roux). Other forms of restrictive surgery includes gastroplasty and sleeve gasrectomy.
Malabsorptive Surgery
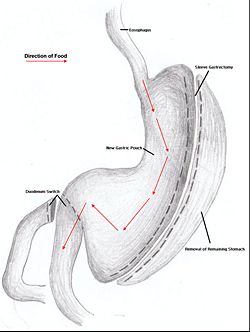
Jejuno-ileal bypass, duodenojejunal bypass and biolopancreatic bypass (with or without duodenal switch)
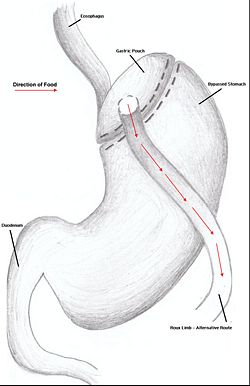
Combination Surgery
Combination surgery combines the benefits of both restrictive and restrictive surgery. The most common bariatric procedure in the US is the Roux-en-Y Gastric Bypass (RYGP).
Duodenal switch
Surgical Effects Regarding Gut Hormones
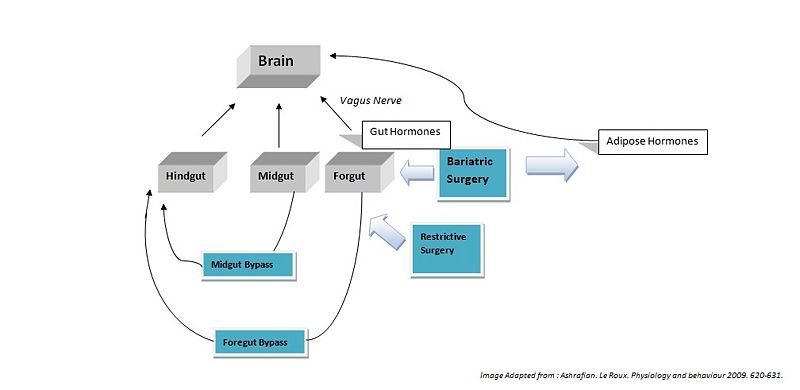
Hindgut Hormones
Peptide tryosine tryosine (PYY) is a peptide beloging to the neuropeptide Y (NPY) family (broberger). PYY is normally released in proportion to carolie intake and has recently been described as an important feedback molecule in the Gut-Brain axis. Following bypass and restrictive surgerys, basal and postprandial PYY levels have been shown to incease (Ashrafian). In addition basal PYY levels have been shown to increase following illial resection and patients have been reported to have lost weight(broberger). As well as being a satiety signal PPY has also been suggested to increase energy expendature(murphy).
Glucagon-like peptide-1 (GLP-1), acts similarly to PYY, acting in the hypothalamus as an anorexigenic signal. The literature shows the majority of patients following foregut bypass surgery show a marked increase in basal and postprandial GLP-1. Midgut bypass also shows an increase in GLP-1 however studies on restrictive surgery have shown either no change or a decrease in GLP-1 basal levels. Of specific interest GLP-1 has been shown to improve postpriandal glycaemic control, being a potent incretin mimetic. A GLP-1 agonist, exenatide has not yet been accepted for use as an anti-obesity drug; however it is already being used in the treatment of type 2 diabetes mellitus.
Midgut Hormones
Neurotensin (NT), is a well know anoregigenic signal where its expression has been shown to be downregulated in ob/ob leptin defficient mice. Following bypass surgerys (5 of 6 reported) have demonstrated an increase in NT levels which could contribute to the anorexigenic effects of the bypass operations.
Foregut Hormones
Ghrelin is an orexigenic hormone (induces hunger)and is released from both the forgut as well as the duodenum. It is released into the blood to promote eating, and levels begin to fall after meals when satiety is reached. Ghrelin is also believed to play a role in regulating body weight over a long period of time. As a result, ghrelin levels increase in order to compensate for the starvation induced by reduced calorie intake observed in diets. However, following bariatric surgery ghrelin levels do not rise as a result of reduced food intake but instead remain low. Therefore, surgery effeciently reduces the appetite stimulating hormone hence lowering the chances of weight being re-gained; as opposed to when high levels of ghrelin are present in the blood during diet induced weight-loss.
Cholecystokinin, Gastrin
Surgical Treatment as Opposed to Diet
Future Possibilites
Conclusion
References
[2]Ashrafian, H. Le roux, C. " Metabolic surgery and gut hormones- A review of bariatric entero-humoral modulation" Physiology and behaviour. (2009) 620-631[1] [3] Broberger, C. "Brain Regulation of food intake and appetite: molecules and networks" Journal of internal Medicine (2005); 258: 301-327.[2] [4]DeMara. "Bariatric Surgery for Morbid Obesity". The new England Journal of Medicine (2007); 356; 2176-83 [3]