Normal weight obesity: Difference between revisions
imported>Sawdah Jakda |
imported>Sawdah Jakda No edit summary |
||
| Line 8: | Line 8: | ||
To clinically classify a person as being obese, their [[Body Mass Index]] (BMI) must be equal to or greater than 30kg/m<sup>2</sup>. However, the spectrum of obesity is quite large. '''Normal Weight Obesity (NWO)''', found in almost half of the American adult population, is when a person has a normal BMI (18.5- 24.9 kg/m<sup>2</sup>) but also has a high percentage of '''body [[adipocyte|fat]]'''(>23.1% for men and >33.3% for women) as well as heart and metabolic disturbances. <ref name=Romero/> | To clinically classify a person as being obese, their [[Body Mass Index]] (BMI) must be equal to or greater than 30kg/m<sup>2</sup>. However, the spectrum of obesity is quite large. '''Normal Weight Obesity (NWO)''', found in almost half of the American adult population, is when a person has a normal BMI (18.5- 24.9 kg/m<sup>2</sup>) but also has a high percentage of '''body [[adipocyte|fat]]'''(>23.1% for men and >33.3% for women) as well as heart and metabolic disturbances. <ref name=Romero/> | ||
Measuring BMI does not take into account muscle or bone mass, and as both are denser than fat, people can have an ‘obese’ BMI while they actually have a healthy percentage of body fat. Conversely, a person can have a normal BMI and be in the normal weight range but have unhealthily high adiposity levels. High percentages of body fat tissue are high risk factors for the diseases and disorders linked to obesity, including diabetes, [[ischemic heart disease]], heart failure, [[hypertension]] and [[sleep apnea]]. <ref name=Burkhauser>Burkhauser R V, Cawley J (2008) Beyond BMI: The value of more accurate measures of fatness and obesity in social science research ''J Health Economics'' 27: 519–29</ref> | Measuring BMI does not take into account muscle or bone mass, and as both are denser than fat, people can have an ‘obese’ BMI while they actually have a healthy percentage of body fat. Conversely, a person can have a normal BMI and be in the normal weight range but have unhealthily high adiposity levels. High percentages of body fat tissue are high risk factors for the diseases and disorders linked to obesity, including diabetes, [[ischemic heart disease]], heart failure, [[hypertension]] and [[sleep apnea]]. <ref name=Burkhauser>Burkhauser R V, Cawley J (2008) Beyond BMI: The value of more accurate measures of fatness and obesity in social science research ''J Health Economics'' 27: 519–29</ref> | ||
== '''Measuring Normal Weight Obesity''' == | == '''Measuring Normal Weight Obesity''' == | ||
| Line 55: | Line 55: | ||
Obesity and fatness are thought to be largely inheritable features <ref name=Farooqi> Farooqi, S. and O’Rahilly, S (2005) MONOGENIC OBESITY IN HUMANS Annu. Rev. Med. 2005. 56:443–58 </ref> <ref>Despre´s JP (2006) Abdominal obesity: the most prevalent cause of the metabolic syndrome and related cardiometabolic riskEuropean Heart Journal Supplements 8: B4–B12</ref> This has been concluded from several family, twin and adoption studies. However, twin studies tend to indicate heritability more so than adoption or family studies. <ref>Maes, H. H. M., Neale, M. C. and Eaves, L. J. (1997) Genetic and Environmental Factors in Relative Body Weight and Human Adiposity. Behavior Genetics, 27: 4</ref> <ref name=Farooqi/> Studies have also recognised genetic variance among fat deposition patterns, showing that some individuals store more fat abdominally than others. Evidence for this comes from studies between monozygotic and dizygotic twins, between biological siblings and adopted siblings and between children living with their biological parents and children living with foster parents. <ref>Hasstedt, S. J., Ramirez, M.E., Kuida,H. and Williams, R. R. (1989) Recessive Inheritance of a Relative Fat Pattern. Am. J. Hum. Genet. 45:917-925</ref> | Obesity and fatness are thought to be largely inheritable features <ref name=Farooqi> Farooqi, S. and O’Rahilly, S (2005) MONOGENIC OBESITY IN HUMANS Annu. Rev. Med. 2005. 56:443–58 </ref> <ref>Despre´s JP (2006) Abdominal obesity: the most prevalent cause of the metabolic syndrome and related cardiometabolic riskEuropean Heart Journal Supplements 8: B4–B12</ref> This has been concluded from several family, twin and adoption studies. However, twin studies tend to indicate heritability more so than adoption or family studies. <ref>Maes, H. H. M., Neale, M. C. and Eaves, L. J. (1997) Genetic and Environmental Factors in Relative Body Weight and Human Adiposity. Behavior Genetics, 27: 4</ref> <ref name=Farooqi/> Studies have also recognised genetic variance among fat deposition patterns, showing that some individuals store more fat abdominally than others. Evidence for this comes from studies between monozygotic and dizygotic twins, between biological siblings and adopted siblings and between children living with their biological parents and children living with foster parents. <ref>Hasstedt, S. J., Ramirez, M.E., Kuida,H. and Williams, R. R. (1989) Recessive Inheritance of a Relative Fat Pattern. Am. J. Hum. Genet. 45:917-925</ref> | ||
The genetic heritability of central obesity is of great interest as the disease is so closely linked to high risk health issues. Genetics cannot be the sole cause of obesity and normal weight obesity, because the human genome has not changed in the recent years that we have seen the dramatic increase in prevalence of disease. However, there are genetic factors which may make some individuals more susceptible to having a higher percentage of body fat. <ref name=Rosmond>Rosmond R (2003) Association studies of genetic polymorphisms in central obesity: a critical review. International Journal of Obesity 27: 1141–1151</ref> Central obesity is more prevalent in males than females and increases with age. Family resemblances have been recognised, suggesting its heritability. Rosmond’s association studies have also shown that abdominal visceral fat levels increase in males and females with age and this increase is not only seen in obese individual but in lean people of normal BMI too. | The genetic heritability of central obesity is of great interest as the disease is so closely linked to high risk health issues. Genetics cannot be the sole cause of obesity and normal weight obesity, because the human genome has not changed in the recent years that we have seen the dramatic increase in prevalence of disease. However, there are genetic factors which may make some individuals more susceptible to having a higher percentage of body fat. <ref name=Rosmond>Rosmond R (2003) Association studies of genetic polymorphisms in central obesity: a critical review. International Journal of Obesity 27: 1141–1151</ref> Central obesity is more prevalent in males than females and increases with age. Family resemblances have been recognised, suggesting its heritability. Rosmond’s association studies have also shown that abdominal visceral fat levels increase in males and females with age and this increase is not only seen in obese individual but in lean people of normal BMI too. | ||
Revision as of 09:57, 15 November 2011
For the course duration, the article is closed to outside editing. Of course you can always leave comments on the discussion page. The anticipated date of course completion is 01 April 2012. One month after that date at the latest, this notice shall be removed. Besides, many other Citizendium articles welcome your collaboration! |
The prevalence of obesity has risen rapidly in recent years and shows no clear signs of slowing down; thus in the USA for example, the prevalence of obesity has increased from ~13% to almost 30% from the 1960s to present time.[1]
To clinically classify a person as being obese, their Body Mass Index (BMI) must be equal to or greater than 30kg/m2. However, the spectrum of obesity is quite large. Normal Weight Obesity (NWO), found in almost half of the American adult population, is when a person has a normal BMI (18.5- 24.9 kg/m2) but also has a high percentage of body fat(>23.1% for men and >33.3% for women) as well as heart and metabolic disturbances. [1]
Measuring BMI does not take into account muscle or bone mass, and as both are denser than fat, people can have an ‘obese’ BMI while they actually have a healthy percentage of body fat. Conversely, a person can have a normal BMI and be in the normal weight range but have unhealthily high adiposity levels. High percentages of body fat tissue are high risk factors for the diseases and disorders linked to obesity, including diabetes, ischemic heart disease, heart failure, hypertension and sleep apnea. [2]
Measuring Normal Weight Obesity
The definition of obese refers to an abnormally high level of adiposity, which means that the metabolic disorders associated with the disease are probably mainly due to the excess in body fat (BF). However, the contemporary way in which to classify someone as obese is by measuring their BMI as they are simple to use and reproduce. Its usage is supported by the fact that high BMI values (clinically obese) correlate with increase in mortality [1].
Although this is the conventional method, the calculations do not differentiate the composition of one’s weight. Body weight can be determined by the lean muscle mass to adipose tissue ratio. Since it has been found that fat cells do not weigh much, it can be very hard to determine whether a person has high levels of body fat using the BMI, especially in those who are not clinically obese (BMI<30kg/m2) [3].
The reason why it is vital to find a better method for defining the obesity spectrum is due to the strong relationship between adiposity and metabolic disorders leading to a high mortality rate. The definition of metabolic syndrome are covered by the following criteria: [1]
| Conditions | Measurements | |
|---|---|---|
| Waist circumference | >102 cm in men and >88 cm in women | |
| HDL | <1.04mmol/L in men and <1.03mmol/L in women | |
| Triglycerides | >1.7mmol/L | |
| Blood Pressure | systolic blood pressure >130mmHg or diastolic blood pressure >85mmHg | |
| Fasting Glucose | >5.5mmol/L |
For the diagnosis of metabolic syndrome, central obesity (waist circumference), along with two other abnormalities must be present. [4]
NWO is observed mainly in middle-aged adults, who have higher BF and lower lean body mass, shown by the increase in fat cell size (FCS). This higher adiposity seen as age increases is thought to be the cause of impairment in glucose tolerance, even in the presence of insulin. This shows that NWO can be characterised by hyperinsulinism and FCS. Offspring studies of patients with hypertriglyceridemia (HTG) show that they could be obese in an unconventional sense even if they are not HTG, as they still display an increased insulin level, proving that NWO is a risk factor for diseases such as type II diabetes. [3]
The suggested cut-off between obesity and NWO is a BMI of 27kg/m2. High circulating levels of insulin were found in patients suffering from coronary heart disease, type II diabetes and other metabolic disorders but this was seen in those that were obese(BMI<28kg/m2) and in patients within the normal range (23-25 kg/m2). Therefore, if BMI is to be used to try and identify those in need of help with adiposity, the cut off points of BMI may need to be revised. [5]
Even though it is hard to measure BF, it would be ideal to find an easy to use test for determining BF as this is what defines obesity. Studies show that there is a fourfold increase in the prevalence of metabolic disorders, dyslipidaemia, hyper tension and cardiovascular diseases (CVD) in patients with a BF greater than 23.1% (men; women > 33.3%) compared to those in the low BF tertile [1]. As an alternative method, it has been suggested that waist circumference measurements be used but the vast range in human error makes it a questionable choice.
It is important to try and identify the patients at risk of developing these metabolic disorders if we are to reduce their mortality rate. Further study needs to be done to identify cut off points of BF% values corresponding to normal and obese. Since in NWO, the BMI is within the normal range, we need to identify those that most at risk from future metabolic complications but at the same time, try and find preventative measures to ensure adiposity levels are controlled. Therefore, the better way to determine the NWO patients from the wider population would be by assessing FCS, insulin levels or waist circumference in place of BMI or BF percentage. [3].
Genetic and Environmental Factors of High Adiposity
High adiposity, specifically in abdominal regions, can serve as a positive indicator of the potential risk of cardiac disease and diabetes mellitus. [6] Both of these diseases along with other conditions are at increased risk when suffering from obesity. This high abdominal adiposity can be independent of body weight, as observed in the normal weight obesity phenotype, and can be evaluated by measuring the waist circumference, or more reliably, the waist-to-hip ratio. [2] As a high percentage of body fat in abdominal regions is closely linked to the health risks of obesity, researching the genetic and environmental causes of the obesity phenotype, central obesity, seems a practical area to look for causes of normal weight obesity.
Obesity and fatness are thought to be largely inheritable features [7] [8] This has been concluded from several family, twin and adoption studies. However, twin studies tend to indicate heritability more so than adoption or family studies. [9] [7] Studies have also recognised genetic variance among fat deposition patterns, showing that some individuals store more fat abdominally than others. Evidence for this comes from studies between monozygotic and dizygotic twins, between biological siblings and adopted siblings and between children living with their biological parents and children living with foster parents. [10]
The genetic heritability of central obesity is of great interest as the disease is so closely linked to high risk health issues. Genetics cannot be the sole cause of obesity and normal weight obesity, because the human genome has not changed in the recent years that we have seen the dramatic increase in prevalence of disease. However, there are genetic factors which may make some individuals more susceptible to having a higher percentage of body fat. [11] Central obesity is more prevalent in males than females and increases with age. Family resemblances have been recognised, suggesting its heritability. Rosmond’s association studies have also shown that abdominal visceral fat levels increase in males and females with age and this increase is not only seen in obese individual but in lean people of normal BMI too.
Currently it is thought that only about 7% of the obese population is affected by monogenic causes of childhood obesity. However, the mutations which cause these forms of obesity are very uncommon. [12] Several genes have been identified as ‘obesity genes’ and although each allele would cause very little variance in BMI alone, a polygenic explanation seems more likely. This means having several high risk alleles might increase the likelihood of obesity in an individual. [13] [11]
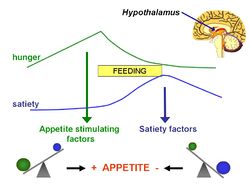
Many of the genes that have been discovered are connected to functions of the hypothalamus and so it is thought that they have a possible role in the balance of energy input and output. However, normal weight obesity is unlikely to be caused or influenced by the same genetic mutations as all other forms of obesity. For instance, the POMC KO causes severe obesity and hyperphagia due to a lack of interactions between melanocortin and the melanocortin 4 receptor. [7] Normal weight obesity phenotype shows a high percentage of body fat in normal weight individuals but no severe obesity and there is unlikely to be any hyperphagia.
Ukkola et al hypothesised that gene interactions between polymorphisms in glucocorticoid receptor, adrenergic receptor and lipoprotein lipase genes have an effect on adiposity and regional fat distribution. Interactions between the genes were observed and have some effects on body fat and its distribution. They also showed that the a2-ADR DraI variant of the adrenergic receptor has been shown to be associated with lower percentage of abdominal body fat. The glucocorticoid receptor gene is also thought to have effects on body fat all over the body. However, the interactions of genes that perhaps influence body fat are very complex and still undefined. [14]
Atherogenic dyslipidemia is a disorder associated with metabolic syndrome with which a sufferer has high triglycerides and low HDL cholesterol. This is often seen in genetic forms of hypercholesterolemia which is quite common. The disease is not typically associated with obesity as there is often no change in energy balance seen and sufferers are typically not obese. Therefore this could be a cause of normal weight obesity and considering that dyslipidemia is associated with an increased risk of cardiovascular disease, more screening for lipid abnormalities needs to be done than simply relying on BMI as an indicator of obesity. [15]
Genetic mutations would not have such a role in central adiposity without the influence of our modern plentiful environment. [6] Environment has to strongly influence the central obesity phenotype as less than 50% of cases are genetically heritable. [11]
Disorders linked to NWO
There are a large number of metabolic complications that result from excess body fat, as well as a number of mechanical complications directly associated with excess body fat (table 1 and 2). Studies involving subjects with normal BMI have reported conflicting findings to the widely held belief; that maintaining a normal weight automatically protects against disorders such as increased adiposity and tendency to develop metabolic syndrome, which often causes type 2 diabetes.
Table 1. Metabolic complications of obesity[16]
| Metabolic complications of obesity |
|---|
| Type 2 diabetes |
| Hypertriglyceridemia/
Low HDL cholesterol |
| Hypertension |
| Non-alcoholic fatty liver disease/
Non-alcoholic steatohepatitis |
| Inflammation |
| Hyperuricemia (excess uric acid) |
| Insulin resistance |
| Polycystic ovarian syndrome |
Table 2. Mechanical complications of obesity[16]
| Mechanical complications of obesity |
|---|
| Gastroesophageal reflux disease |
| Obstructive sleep apnea |
| Degenerative joint disease |
The effect of free fatty acids (FFA) on glucose metabolism in humans has been studied extensively. Studies have established that obesity and increased plasma FFA concentrations are risk factors for the development of type 2 diabetes. Elevated plasma FFA concentrations upregulate glucose production and impair muscle glucose uptake, oxidation and storage. Increased insulin release can also result, as well as pancreatic beta-cell dysfunction.
In addition to their effects on glucose metabolism and risk of diabetes, increased FFA concentrations have been shown to be associated with ischemic heart disease. [16]
To support this increase in insulin secretion, another study showed that adult-onset NWO individuals show hyperinsulinism, and also an increase in fat cell size, compared to obese patients of similar age, height and weight. The subjects in this study also showed hypertriglyceridemia, which is associated with HDL deficiency, atherosclerosis and pancreatitis. [5]
Hypertension and cholesterol cholelithiasis are also associated with obesity, and can also result in NWO individuals. These conditions have been shown to improve with caloric restriction both in obese and NWO patients. It is still not clear how subtle increases in adiposity and/or hyperinsulinism cause pathogenesis of obesity-related metabolic complications in normal weight individuals.[5]
Early inflammation and greater proinflammatory cytokine levels in plasma is also characterized in NWO women, compared to non-obese women. White body fat, or adipose tissue, is functionally similar to dynamic endocrine organ; it secretes various adipokines including proinflammatory factor, such as TNF-alpha, IL-6 and IL-1. Since they play an essential role in the onset of cardiovascular disease, atherosclerotic processes and insulin resistance, this supports the concept that NWO patients may be predisposed to develop metabolic syndrome and CV disease.[1]
Romero-Corral et al. reported that NWO is strongly associated with cardiometabolic dysregulation and a high prevalence of metabolic syndrome in these individuals is similar to that in overweight subjects. The study shows that in women, NWO is independently associated with an increased risk for CV mortality. They also found a correlation between increased waist circumference (>87cm in men and >82cm in women) and CV risk, which is a similar correlation observed with BF%. Since devices for measuring BF are not widely available in clinical practice, this study reinforces the reliability of waist circumference measurement as an alternative method of prognosis, which is easier and inexpensive.[1]
These studies show that a focus on maintaining "a healthy weight" may need to be shifted to maintaining "a healthy body fat percentage". It is important to be aware that even people with normal weight may have excessive body fat, and that they may be at risk of developing diabetes and heart disease.
Treatment and Prevention
As mentioned previously NWO is classified as having a healthy BMI, but a high percentage of fat. Therefore to effectively manage NWO, the main aim is to prevent the problems associated with NWO, such as type 2 diabetes, hypertension, hypertriglyceridemia and cardiovascular diseases. However if these associated symptoms of NWO are existing, then the aim is to control and prevent any further progression of these conditions. As well as pharmalogically treating the specific conditions, by taking antihypertensive drugs for example, diet and exercise are also very effective at controlling and treating NWO.
For individuals who are overweight and obese, the best treatment is to lose weight through a very low calorie diet. Whereas NWO individuals should be placed on a calorie controlled diet, but not as calorie restrictive as overweight/obese individuals, this will lead to a reduction in adipose tissue mass and prevent a further increase in adiposity. Calorific restriction also alleviates the associated insulin resistance[3]. Ruderman et al(2011) found a 4-12 week calorie restricted diet to be successful in treating NWO, and is some cases was the only therapy needed to treat NWO[5]. A well balanced diet is also needed, for example high carbohydrate diet increases the risk of hyperinsulinism in NWO, therefore eating a low carbohydrate is beneficial. A Diet high in folic acid, B12, and antioxidants will protect against the development of cardiovascular diseases.
Through regular exercise muscle mass will increase, and lead to a reduction in fat stores, leading to a healthier BMI, with healthier adiposity levels. Exercise is of great benefit for NWO individuals as it improves insulin sensitivity[5]. Ruderman et al (1981) state that exercise decreases triglycerides levels, thus decreasing the risk of high cholesterol associated diseases and diabetes. A further benefit of exercise is that it increases high density lipoproteins. Hypertension associated with NWO can be treated with exercise which lowers blood pressure.[3]
The best treatment for NWO is through combining a low calorie diet with regular exercise. NWO Individuals with abnormal glucose tolerance showed a 30-50% reduction in developing type 2 diabetes, and glucose tolerance returned to normal through combinational therapy, compared to diet alone with no exercise, thus demonstrating the importance of regular exercise for treating NWO.[5]
If exercise and diet do not work, then pharmacological approaches should be used. For example, thiazolidinediones are successful in treating abnormal insulin sensitivity. In addititon, anorexigenic drugs can treat NWO as they cause significant weight loss and prevent the onset of type 2 diabetes. Statins can be used to lower cholesterol levels, thus reducing the risk of cardiovascular diseases, whilst to lower blood pressure antihypentensives can be used.[5]
The conditions associated with NWO such as hypertension can have dangerous consequences, therefore it would be ideal to identify people at risk of NWO earlier, so diet and exercise regimes could be advised in order to prevent any further progression, in which genetic markers would be effective to establish individuals at risk.[5]
Conclusion
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Romero-Corral A et al. (2010) Normal weight obesity: a risk factor for cardiometabolic dysregulation and cardiovascular mortality Eur Heart J 31:737-46 PMID 19933515
- ↑ 2.0 2.1 Burkhauser R V, Cawley J (2008) Beyond BMI: The value of more accurate measures of fatness and obesity in social science research J Health Economics 27: 519–29
- ↑ 3.0 3.1 3.2 3.3 3.4 Ruderman NB, Schneider SH, Berchtold P, (1981) The "metabolically-obese," normal weight individual, The American Journal of Clinical Nutrition 34, 1617-1621
- ↑ Sir George Alberti, Paul Zimmet, Jonathan Shaw and Scott M. Grundy (2006). the IDF consensus worldwide definition of the metabolic syndrome. Belgium: International Diabetes Federation.pg 10
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 Ruderman N, Chisholm D, Pi-Sunyer X, Schneider S (1998) The metabolically obese, normal-weight individual revisited Diabetes 47:699–713
- ↑ 6.0 6.1 Despre´s JP (2006) Abdominal obesity: the most prevalent cause of the metabolic syndrome and related cardiometabolic riskEuropean Heart Journal Supplements 8: B4–B12
- ↑ 7.0 7.1 7.2 Farooqi, S. and O’Rahilly, S (2005) MONOGENIC OBESITY IN HUMANS Annu. Rev. Med. 2005. 56:443–58
- ↑ Despre´s JP (2006) Abdominal obesity: the most prevalent cause of the metabolic syndrome and related cardiometabolic riskEuropean Heart Journal Supplements 8: B4–B12
- ↑ Maes, H. H. M., Neale, M. C. and Eaves, L. J. (1997) Genetic and Environmental Factors in Relative Body Weight and Human Adiposity. Behavior Genetics, 27: 4
- ↑ Hasstedt, S. J., Ramirez, M.E., Kuida,H. and Williams, R. R. (1989) Recessive Inheritance of a Relative Fat Pattern. Am. J. Hum. Genet. 45:917-925
- ↑ 11.0 11.1 11.2 Rosmond R (2003) Association studies of genetic polymorphisms in central obesity: a critical review. International Journal of Obesity 27: 1141–1151
- ↑ Frayling, T. M. et al (2007)A Common Variant in the FTO Gene Is Associated with Body Mass Index and Predisposes to Childhood and Adult Obesity Science. 316(5826): 889–894
- ↑ Hofker M & Wijmenga C (2009) A supersized list of obesity genes nature genetics 41: 2
- ↑ Ukkola, O, Pe´russe, L, Chagnon, YC, Despre´s J-P, Bouchard C (2001) Interactions among the glucocorticoid receptor, lipoprotein lipase and adrenergic receptor genes and abdominal fat in the Que´bec Family Study International Journal of Obesity 25, 1332–1339
- ↑ Daniels S. R, (2011) Lipid concentrations in children and adolescents: it is not all about obesity. The American Journal of Clinical Nutrition. 94:699–700
- ↑ 16.0 16.1 16.2 Jensen M.(2009) Normal weight obesity. International Chair on Cardiometabolic Risk 2(1), 23-30
- ↑ Ruderman "et al" (1981) The "metabolically-obese," normal weight individual, The American Journal of Clinical Nutrition 34, 1617-1621