Syphilis: Difference between revisions
imported>Howard C. Berkowitz No edit summary |
imported>Howard C. Berkowitz No edit summary |
||
| Line 1: | Line 1: | ||
{{subpages}} | |||
{{Infobox_Disease | | {{Infobox_Disease | | ||
Name = Syphilis | | Name = Syphilis | | ||
Revision as of 00:54, 31 January 2009
| Syphilis | |
|---|---|
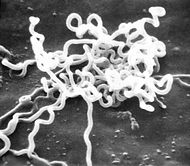
| Treponema pallidum spirochete | |
| MedlinePlus | 001327 |
| MeSH | D013587 |
In medicine, syphilis is a "contagious venereal disease caused by the spirochete treponema pallidum."[1]
Stages of syphilis
Syphilis is an unusual infectious disease because this illness is qualitatively different at different stages of infection. There are 3 such stages, and the disease is accordingly named: primary, secondary, and tertiary syphilis. Without treatment, syphilis is marked by periods of acute symptoms, followed by latent periods. Those latent periods often delude the infected person into believing that whatever was wrong has now healed or passed, because most or all of the symptoms or signs that flared in the acute period disappear on their own. Despte that, the infection does not go away without treatment and the disease progresses from the first, to the second, and then to the third stage.
Although antibiotic treatment is effective for early syphilis, tertiary syphilis is not easily eradicated and is often associated with permanent damage, whether or not the infecting organisms can be completely banished from the body. In some ways, these features of syphilis are similar to another spirochete infection, one that is not venereal in nature but spread by the bite of infected ticks, Lyme disease. The spirochete that causes syphilis, Treponemum pallidum pallidum, is one of two subspecies of T. pallidum that causes human disease. T. pallidum can push its way through the unbroken mucosa of the genital tract and of the inner nose, lips, oral cavity, and throat, and can also enter the body through microscopic breaks in skin.

Early syphilis
Early syphilis includes both the primary and secondary stages. During this time the disease is easily passed to sexual contacts, and is also easily curative with the proper antibiotic treament. The signs and symptoms of early syphilis will go away by themselves without treatment, but the infection will not. Instead the disease will progress to the late stage in which treatment does not reliably produce a cure. For both selfish and altruistic reasons, a person who may possiby have syphilis is best tested for the infection as soon as possible. In many countries and regions within nations, such tests are carried out routinely during the prenatal care of pregnant women, and upon admission to the hospital or application for marriage licenses.
Primary syphilis
The lesions of primary syphilis do not appear immediately after the infection is contracted. The infecting organism, the spirochete T. pallidum enters the new host's body (either through intact mucosa or a small break in the skin) and then begins to reproduce in the superficial tissues near the entry site. After about two to six weeks from the that time, that area of skin or mucosa will show lesion or lesions: usually a painless nodule. The lesion of primary syphilis is called a chancre. This nodule, a round thickening of tissue, may ulcerate and appear to be an open wound, or the nodules may be multiple, in some cases, they have a wart-like appearance rather than appearing smooth. Physicans describe regional enlargement of lymph nodes that occurs along with the appearance of this primary lesion, but the lymph node enlargement is also painless - and may not be noticed by the afflicted person. Regional lymph nodes drain the part of the body that is infected with the primary chancre of syphilis and enlarge because they also become secondarily infected. Their location in the body depends on the location of the lesion. If the chancre is on the lip, the lymph nodes that enlarge will be in the neck. Chancres are usually on the genitals, and so, the enlarged lymph nodes are ordinarily in the groin ("inguinal adenopathy)". However, the primary lesion of syphilis can appear anywhere on the body that had an area that contacted the other person's reservoir of infection and allowed entry of the spirochete through a break in the skin. If that area was a finger, for example, the enlarged lymph nodes will be under the arm- the axillary lymph nodes.
Secondary syphilis

Late syphilis
In late syphilis, disease is sequestered in various parts of the infected person's body. Although a pregnant woman with active tertiary syphilis will likely have a baby born with congenital syphilis, late stage syphilis is not easily passed to sexual contacts. There are many erosions and lesions that are possible throughout the body, ranging from deafness from involvement of the bone surrounding the inner ear, to large ulcers deforming the face and other visible parts of the external body, to heart disease, to brain and central nervous system involvement which may cause dementia and mental illness. Some of these impairments and lesions will heal with treatment, but many- such as los of mental and hearing acuity, are not completely recovered despite treatment. Without treatment, some forms of tertiary syphilis are fatal.
The externally visible lesions of late (tertiary) syphilis is called a gumma. [2]
Congenital syphilis
Although the great majority of cases of syphilis are contracted through sex, infants born to untreated mothers with either primary, secondary or tertiary syphilis may be infected. This type of syphilis is known as congenital syphilis, and it is a leading cause of stillbirths and death among newborns and young infants in many developing countries. In developed countries, blood tests for syphilis are a routine part of prenatal care.
The incidence of congenital syphilis" is a lower, but parallel, incidence of the infectious syphilis in females. In the USA, "the number of reported cases of congenital syphilis in infants 1 year of age was lowest (107 cases) in 1978, when infectious syphilis was most prevalent among homosexual and bisexual men. The dramatic increase in the incidence of primary and secondary syphilis among women from 1986 to 1990 resulted in a proportionate increase in the number of infants born with congenital syphilis—to 4424 infants in 1991. The incidence of early syphilis among women has declined since 1991, as has the number of reported cases of congenital syphilis in infants (with 529 cases in 2000). It is important to note that the case definition for congenital syphilis was broadened in 1989 and now includes all live or stillborn infants delivered to women with untreated or inadequately treated syphilis at delivery." (reference for quote:Sheila A. Lukehart. Chapter 153. "Syphilis" in Dennis L. Kasper, Eugene Braunwald, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, and Kurt J. Isselbacher, Eds.Harrison's Principles of Internal Medicine, 16th Edition)Before that time, cases were only counted if the infant was diagnosed with the infection. Now, if the mother has the infection and has not been adequately treated, infants are resumed to be infected as well.
Diagnosis
Recently, the United States Centers for Disease Control and Prevention suggested that some clinical laboratories reverse the usual sequency of tests used for diagnosing syphilis and now use the more expensive, treponemal test first before the nontreponemal test.[3]
Treatment
Penicillin remains the mainstay of the modern treatment of syphilis; T. pallidum has not developed significant resistance.
Syphilis in historical perspective
As far as recorded history is concerned, syphilis made its debut in 15th century Europe. Whether it came from the sailors returning from the new world, or from a new strain of a locally established organism (related to the spirochete of a similar species that causes yaws) is unknown. What is known is that "the great pox" began and, by the 17th century, epidemics of syphilis had not only spread through the population of Europe but had been carried by travelling Europeans to other areas of the world. In this early era of syphilis that disease was as devastating to the populations it infected as a later epidemic of a sexually transmitted illness, AIDS, has been. Until the discovery of antibiotics, the incidence and prevalence of syphilis rose dramatically after every war, beginning with the Neopolonic and ending with War World II. Public education and treatment with penicillin have both been important in changing this pattern.
In the pre-antibiotic era, when toxic heavy metal containing compounds were the only effective remedies for the dread venereal disease, syphilis, the standing joke among medical students was " one night on Venus and the rest of your life on Mercury". These compounds did kill the spirochete, and sometimes cured the syphilis infection, but also made the patient sick and sometimes caused life long side effects, whether or not the syphilis was cured.
By the middle of the 20th century, the treatment situation suddenly changed and syphilis became easily curable- at least in its early stages. Penicillin, along with sex education, changed the demographics of the disease. In the United States, because of "widespread screening and treatment by the Surgeon General Thomas Parran after the Second World War, reported cases of primary and secondary syphilis dropped to an all-time low in 1955." However, rates did rise again, and have shown a 10-year cycle of rising and falling in a fairly regular fashion.
"In North America and the developed countries of northern Europe, syphilis had become predominately a disease of homosexual men by the 1970s. During the late 1980s, there were renewed outbreaks of heterosexual and congenital syphilis in North America in the wake of the HIV epidemic."(George R Kinghorn Chapter 75 – Syphilis in Cohen & Powderly: Infectious Diseases, 2nd ed. copyright 2004). That epidemic ended, to be replaced, in terms of global infection, with a large increase in cases in Eastern Europe and parts of Asia. In the Soviet Union (1918–1992), public health, including sexually transmitted disease (STD) control, was carefully monitored, with rights of personal freedom and privacy secondary to the control of disease. These strict and enforced measures controlled syphilis in the USSR. The incidence of syphilis never exceeded 40 cases per 100,000 in St. Petersburg, during the soviet regime. The collapse of the USSR in the early 1990s caused not only a collapse of the syphilis control program, but a fundamental change in the economic, social, and psychologic makeup of life in Russia. This period marked the rise of a Russian syphilis epidemic.
Tuskegee Syphilis Study
The Tuskegee Syphilis Study was an important issue in medical ethics.
References
- ↑ Anonymous (2024), Syphilis (English). Medical Subject Headings. U.S. National Library of Medicine.
- ↑ Beerman Nicholas L. Late syphilis: a review of some of the recent literature. American Journal of the Medical Sciences. 254(4):549-69, 1967 Oct. PMID 4862998
- ↑ Anonymous (August 15, 2008). Syphilis Testing Algorithms Using Treponemal Tests for Initial Screening --- Four Laboratories, New York City, 2005--2006. Centers for Disease Control and Prevention. Retrieved on 2008-11-20.