Chordoma: Difference between revisions
imported>Daniel Mietchen |
imported>Daniel Mietchen |
||
| Line 15: | Line 15: | ||
==Diagnostics== | ==Diagnostics== | ||
Chordomas are most frequently identified on the basis of [[MRI|MRI scans]]. They can also, with lower probability, be identified on [[CT scan]], particularly if the tumour has grown considerably. [[Histology|Histologically]], chordomas can be identified using a variety of [[immunohistochemical]] markers. | Chordomas are most frequently identified on the basis of [[MRI|MRI scans]]. They can also, with lower probability, be identified on [[CT scan]], particularly if the tumour has grown considerably. [[Histology|Histologically]], chordomas can be identified using a variety of [[immunohistochemical]] markers. | ||
{{Image|Chordoma immunohistochemistry.png|right|250px|Different [[immunohistochemical marker]]s of chordoma. A: [[Ethyl eosin]] staining of a chordoma composed of nests and cords of tumour cells; B: Ethyl eosin staining of [[physaliphorous cell]]s containing multiple clear [[cytoplasm]]ic [[vacuole]]s; C: [[immunohistochemistry]] showing staining for [[S-100 protein]]; D: immunohistochemistry showing staining for [[cytokeratin]]; E: immunohistochemistry showing staining for [[Epithelial membrane antigen|EMA]]; F: immunohistochemistry showing staining for [[Vimentin]]. Scale: Panel A is 6. | {{Image|Chordoma immunohistochemistry.png|right|250px|Different [[immunohistochemical marker]]s of chordoma. A: [[Ethyl eosin]] staining of a chordoma composed of nests and cords of tumour cells; B: Ethyl eosin staining of [[physaliphorous cell]]s containing multiple clear [[cytoplasm]]ic [[vacuole]]s; C: [[immunohistochemistry]] showing staining for [[S-100 protein]]; D: immunohistochemistry showing staining for [[cytokeratin]]; E: immunohistochemistry showing staining for [[Epithelial membrane antigen|EMA]]; F: immunohistochemistry showing staining for [[Vimentin]]. Scale: Panel A is 6.4 mm wide, all others 1.6 mm.}} | ||
==Therapy== | ==Therapy== | ||
Revision as of 07:58, 13 May 2010
A chordoma (also known as choroid meningioma, chordocarcinoma, chordoepithelioma, or notochordoma) is a malignant tumor arising from the embryonic remains of the notochord.[1]
Etymology
The term derives — in analogy of carcinoma — from the Latin word chorda for string and the Greek suffix -oma designating a swelling.
Etiology
Chordomas are the result of dysregulation in remnants of the notochord. As such, they can occur anywhere in the bony tissue surrounding the spinal cord, with cranial, thoraco-lumbal and sacral tumours each representing about one third of the cases.
Demographics
The prevalence is about 1 in a million in the United States, and affected patients have an average life expectancy of five to ten years after diagnosis, with differences according to age of onset, gender and ethnicity.[2]
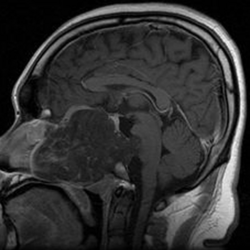
Diagnostics
Chordomas are most frequently identified on the basis of MRI scans. They can also, with lower probability, be identified on CT scan, particularly if the tumour has grown considerably. Histologically, chordomas can be identified using a variety of immunohistochemical markers.

Different immunohistochemical markers of chordoma. A: Ethyl eosin staining of a chordoma composed of nests and cords of tumour cells; B: Ethyl eosin staining of physaliphorous cells containing multiple clear cytoplasmic vacuoles; C: immunohistochemistry showing staining for S-100 protein; D: immunohistochemistry showing staining for cytokeratin; E: immunohistochemistry showing staining for EMA; F: immunohistochemistry showing staining for Vimentin. Scale: Panel A is 6.4 mm wide, all others 1.6 mm.
Therapy
At least one susceptibility gene has been identified[3] but currently, no therapy is in sight. This leaves surgery as the main option of treatment, with prospects of success varying according to location.
References
- ↑ Anonymous (2025), Chordoma (English). Medical Subject Headings. U.S. National Library of Medicine.
- ↑ McMaster ML, Goldstein AM, Bromley CM, Ishibe N, Parry DM (2001). "Chordoma: incidence and survival patterns in the United States, 1973-1995". Cancer Causes Control 12 (1): 1-11. DOI:10.1023/A:1008947301735. PMID 11227920. Research Blogging. [e]
- Reports on a long-term study involving 400 patients with microscopically confirmed chordoma, revealing an overall prevalence of about 1 per million in the United States and a median survival time of about 6 years after diagnosis. It also shows that cranial, spinal and sacral locations each represent about one third of the total number of cases, and that males are affected about twice as often as females.
- ↑ Yang XR, Ng D, Alcorta DA, Liebsch NJ, Sheridan E, Li S et al. (2009). "T (brachyury) gene duplication confers major susceptibility to familial chordoma". Nat Genet 41 (11): 1176-8. DOI:10.1038/ng.454. PMID 19801981. Research Blogging. [e]
- Based on comparative genomic hybridization data from four affected families, variations in the 6q27 region of the human chromosome 6 were found to be correlated with chordoma, thus suggesting the T gene as a potential susceptibility gene for the disease.