Influenza
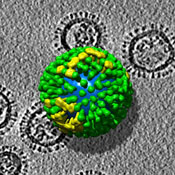
Influenza, commonly called “the ‘Flu”, is described as "an acute viral infection in humans involving the respiratory tract. It is marked by inflammation of the nasal mucosa; the pharynx; and conjunctiva, and by headache and severe, often generalized, myalgia".[1] It is contagious (easily passed from one person to another) and is caused by viruses of the Orthomyxoviridae family.
Hosts
Influenza in humans
Symptoms of Influenza include headache, coughing and other cold-like symptoms. These are accompanied by a high fever. The flu is easily treated with modern medicines, but many strains are nevertheless quite serious, particularly for children and older persons.
Equine Influenza
This is a species-specific strain that infects horses, ponies, donkeys and mules. Humans do not catch this disease but are carriers of it. It is airborne and highly contagious. Equine influenza generally does not kill its victims, and affected horses display similar symptoms to those of humans.
In 2007, a horse flu epidemic began in New South Wales, Australia. The outbreak is believed to have begun as a result of infractions of proper quarantine procedure and is expected to cost millions of dollars in lost revenue. As of September, 2007, it had spread to the Victorian border, causing the cancellation of events at the Melbourne Show, and the possibility that the Spring Carnival, including the running of the Melbourne Cup horse race, would be canceled.
Avian flu
Avian flu, also known as Bird flu or H5N1, has led to recent outbreaks.[2][3]
Epidemiology
Google maintains statistics based on search terms (http://www.google.org/flutrends/).[5]
The prevalence of influenza among people who have an "influenza-like illness" varies strongly with the seasons of the year. In the United States, the Centers for Disease Control and Prevention (CDC) maintains public statistics at http://www.cdc.gov/flu/weekly/fluactivity.htm.
- During the off season, the the prevalence is < 2%[4]
- During the height of season, the prevalence may be 20-35%.[4]
- During local outbreaks, the prevalence may be 50-80% according to studies.[6][7] Unfortunately, the CDC does not report sufficient details to determine where local outbreaks are occurring.
In addition to seasonal variations, there have been several worldwide influenza epidemics, resulting in millions of deaths.
Diagnosis
History and physical examination
Since anti-viral drugs are effective in treating influenza if given early (see treatment section, below), it can be important to identify cases early. A systematic review by the Rational Clinical Examination concluded that the best findings for excluding the diagnosis of influenza are:[8]
| Finding: | Sensitivity | Specificity |
|---|---|---|
| Fever† | 86%† | 25% |
| Cough† | 98%† | 23% |
| Nasal congestion† | 70–90%† | 20–40% |
| Absence of vaccination | 83-97% | 14-19%[9][10] |
| Note: † All three findings, especially fever, were less sensitive in patients over 60 years of age.[8] | ||
Using the symptoms listed above, the combinations of findings below can improve diagnostic accuracy.[11] Unfortunately, even combinations of findings are imperfect. However, Bayes Theorem can combine pretest probability with clinical findings to adequately diagnose or exclude influenza in some patients. The pretest probability has a strong seasonal variation; the current prevalence of influenza among patients in the United States receiving sentinel testing is available at the CDC.[12] Using the CDC data, the following table shows how the likelihood of influenza varies with prevalence:
| Combinations of findings | Sensitivity | Specificity | Projected during local outbreaks (prevalence approx 66%[13][7]) |
Projected during influenza season (prevalence=25%) |
Projected in off-season (prevalence=2%) |
|||
|---|---|---|---|---|---|---|---|---|
| PPV | NPV | PPV | NPV | PPV | NPV | |||
| Fever and cough | 64% | 67% | 79% | 49% | 39% | 15% | 4% | 1% |
| Fever and cough and sore throat | 56 | 71 | 79 | 45 | 39 | 17 | 4 | 2 |
| Fever and cough and nasal congestion | 59 | 74 | 81 | 48 | 43 | 16 | 4 | 1 |
Laboratory tests
Rapid tests include immunofluorescence assays, immunoenzyme technique, and polymerase chain reaction testing. The sensitivity of these tests range from 63% to 95%.[14][15]
Differential diagnosis
Influenza-like illness is defined as "fever (temperature of 100°F [37.8°C] or greater) and a cough and/or a sore throat in the absence of a known cause other than influenza."[16] A study from Australia found that possible causes for influenza-like illness include respiratory syncytial virus, rhinovirus, adenovirus, parainfluenza viruses, coronaviruses, and metapneumovirus.[17]
Other diagnoses to consider are:
- Parvovirus B19 - arthropathy is prominent
- Flaviviruses
- Dengue fever - bonebreak fever with retro-orbital pain
- West Nile virus - tremor is common
Treatment
The two classes of anti-virals are neuraminidase inhibitors and M2 inhibitors (adamantane derivatives). Neuraminidase inhibitors are currently preferred for flu virus infections.
Different strains of influenza virus have differing degrees of resistance against these antivirals and it is impossible to predict what degree of resistance a future pandemic strain might have.[18]
When to treat
According to two decision analysis studies of adults, treatment may be justified in the following settings:
- Elderly patients if the probability of influenza is over 14%[7]
- Adults if the probability of influenza is over 30%[6].
During local outbreaks of influenza, the prevalence will be over 50-80%[13][7] and thus patients with any of the above combinations of symptoms may be treated with neuramidase inhibitors without testing. In the absence of a local outbreak, treatment may be justified in the elderly during the influenza season as long as the prevalence is over 15%.[7]
Neuraminidase inhibitors
These drugs are often effective against both influenza A and B.[19] Examples are oseltamivir (trade name Tamiflu) and zanamivir (trade name Relenza) are neuraminidase inhibitors.[20] The Cochrane Collaboration concluded that these drugs reduce symptoms and complications.[21] Zanamivir may cause bronchospasm in patients with asthma.
M2 inhibitors (adamantanes)
These drugs are sometimes effective against influenza A if given early in the infection, but are always ineffective against influenza B. Examples include the antiviral drugs amantadine and rimantadine which block a viral ion channel and prevent the virus from infecting cells. [19]
Prevention
Vaccination
In the United States, the Centers for Disease Control and Prevention has published recommendations on who should get the influenza vaccination.[22] Protection from infection occurs by two weeks after vaccination and lasts one year.[22]
Neuraminidase inhibitors
The Cochrane Collaboration has concluded that neuraminidase inhibitors can prevent symptomatic influenza.[21] Zanamivir may cause bronchospasm in patients with asthma. In addition, oseltamivir may reduce the incidence of respiratory complications on one of 13 patients who take it (number needed to treat = 13).[23] This trial only included patients up to 65 years old.
History
Spanish influenza pandemic of 1918
A pandemic of Spanish Influenza swept across Europe in the wake of the Great War (1918-19). More people are believed to have died of the flu in the year after the war then in the Great War itself. Estimates vary but it is estimated that one third of the world's population were infected and up to 50 million people perished in this pandemic (it is possibly that fatalities world wide were as high as 100 million).[24] Some comparisons are drawn between Spanish Flu and the Black Death (Bubonic Plague) of 1347 to 1351. Estimates are that the flu killed more people in one year than plague did in four.
In the United States, the epidemic led to closing of schools and banning of public meetings in order to successfully reduce mortality.[25]
References
- ↑ National Library of Medicine. "Influenza". [e]
- ↑ Oner AF, Bay A, Arslan S, et al (2006). "Avian influenza A (H5N1) infection in eastern Turkey in 2006". N. Engl. J. Med. 355 (21): 2179–85. DOI:10.1056/NEJMoa060601. PMID 17124015. Research Blogging.
- ↑ Kandun IN, Wibisono H, Sedyaningsih ER, et al (2006). "Three Indonesian clusters of H5N1 virus infection in 2005". N. Engl. J. Med. 355 (21): 2186–94. DOI:10.1056/NEJMoa060930. PMID 17124016. Research Blogging.
- ↑ 4.0 4.1 4.2 Centers for Disease Control and Prevention. Flu Activity. Retrieved on 2007-11-29.
- ↑ Helft M (Nov 11, 2008). Google Uses Web Searches to Track Flu’s Spread - NYTimes.com. New York Times Company. Retrieved on 2008-11-11.
- ↑ 6.0 6.1 Smith K, Roberts M (2002). "Cost-effectiveness of newer treatment strategies for influenza.". Am J Med 113 (4): 300-7. DOI:10.1016/S0002-9343(02)01222-6. PMID 12361816. Research Blogging.
- ↑ 7.0 7.1 7.2 7.3 7.4 Rothberg M, Bellantonio S, Rose D (2003). "Management of influenza in adults older than 65 years of age: cost-effectiveness of rapid testing and antiviral therapy.". Ann Intern Med 139 (5 Pt 1): 321-9. PMID 12965940.
- ↑ 8.0 8.1 8.2 8.3 Call S, Vollenweider M, Hornung C, Simel D, McKinney W (2005). "Does this patient have influenza?". JAMA 293 (8): 987-97. DOI:10.1001/jama.293.8.987. PMID 15728170. Research Blogging.
- ↑ Hulson TD, Mold JW, Scheid D, et al (December 2001). "Diagnosing influenza: the value of clinical clues and laboratory tests". J Fam Pract 50 (12): 1051–6. PMID 11742606. [e]
- ↑ van Elden LJ, van Essen GA, Boucher CA, et al (August 2001). "Clinical diagnosis of influenza virus infection: evaluation of diagnostic tools in general practice". Br J Gen Pract 51 (469): 630–4. PMID 11510391. PMC 1314072. [e]
- ↑ Monto A, Gravenstein S, Elliott M, Colopy M, Schweinle J (2000). "Clinical signs and symptoms predicting influenza infection.". Arch Intern Med 160 (21): 3243–7. PMID 11088084.
- ↑ Centers for Disease Control and Prevention. Weekly Report: Influenza Summary Update. Accessed January 1, 2007.
- ↑ 13.0 13.1 Smith K, Roberts M (2002). "Cost-effectiveness of newer treatment strategies for influenza.". Am J Med 113 (4): 300-7. DOI:10.1016/S0002-9343(02)01222-6. PMID 12361816. Research Blogging.
- ↑ Beyer WE. Heterogeneity of case definitions used in vaccine effectiveness studies--and its impact on meta-analysis. Vaccine. 2006 Nov 10;24(44-46):6602-4. Epub 2006 Jun 8. PMID 16797799
- ↑ Rodriguez WJ, Schwartz RH, Thorne MM. Evaluation of diagnostic tests for influenza in a pediatric practice. Pediatr Infect Dis J. 2002 Mar;21(3):193-6. PMID 12005080
- ↑ Centers for Disease Control and Prevention (2007). CDC - Influenza (Flu) - Flu Activity. Retrieved on 2007-11-19.
- ↑ Kelly H, Birch C (2004). "The causes and diagnosis of influenza-like illness". Australian family physician 33 (5): 305–9. PMID 15227858. [e]
- ↑ Webster, Robert G. (2006). "H5N1 Influenza — Continuing Evolution and Spread". N Engl J Med 355 (21): 2174–77. PMID 16192481.
- ↑ 19.0 19.1 Stephenson, I; Nicholson K (1999). "Chemotherapeutic control of influenza". J Antimicrob Chemother 44 (1): 6–10. PMID 10459804.
- ↑ Moscona, A (2005). "Neuraminidase inhibitors for influenza". N Engl J Med 353 (13): 1363–73. PMID 16192481.
- ↑ 21.0 21.1 Jefferson, T; Demicheli V, Di Pietrantonj C, Jones M, Rivetti D. "Neuraminidase inhibitors for preventing and treating influenza in healthy adults". Cochrane Database Syst Rev 3: CD001265. DOI:10.1002/14651858.CD001265.pub2. PMID 16855962. Research Blogging.
- ↑ 22.0 22.1 Centers for Disease Control and Prevention. CDC - Influenza (Flu): Vaccination. Retrieved on 2007-11-29.
- ↑ Treanor JJ, Hayden FG, Vrooman PS, et al (2000). "Efficacy and safety of the oral neuraminidase inhibitor oseltamivir in treating acute influenza: a randomized controlled trial. US Oral Neuraminidase Study Group". JAMA 283 (8): 1016–24. PMID 10697061. [e]
- ↑ http://www.cdc.gov/ncidod/EID/vol12no01/05-0979.htm
- ↑ Markel H, Lipman HB, Navarro JA, et al (2007). "Nonpharmaceutical interventions implemented by US cities during the 1918-1919 influenza pandemic". JAMA 298 (6): 644–54. DOI:10.1001/jama.298.6.644. PMID 17684187. Research Blogging.