Rabies virus
| Rabies Virus | ||||||||
|---|---|---|---|---|---|---|---|---|
 | ||||||||
| Scientific classification | ||||||||
|
Description and significance
The Rabies virus is a member of the order, Mononegavirales, which encompasses viruses containing non-segmented, negative-stranded RNA genomes.[1] The term originates from the Latin, “rabies,” which means “madness.” This may have been derived from the Sanskrit word, rabhas, “to do violence.” The virus has a distinct “bullet” shape, placing it in the Rhabdoviridae family, which includes at least three genera of viruses that infect animals, such as Lyssavirus, Ephemerovirus, and Vesiculovirus. The rabies virus belongs to the Lyssavirus genus (Greek word, lyssa, is derived from “lud” or “violent.”) which also includes the Aravan virus, Australian bat Lyssavirus, Duvenhage virus, European bat viruses 1 and 2, Lagos bat virus, and Mokola virus. Lyssaviruses have helical symmetry and are about 180 nm in length, with a cross-sectional diameter of 75 nm.[2] The most prevalent strain of rabies is Rabies Virus (RABV; genotype 1), which is the type that infects both bats in the Americas and terrestrial animals throughout the world. Rabies is a zoonotic disease, meaning it is transmitted from animals to humans. The virus infects domestic and wild animals, and is transmitted to humans through close contact with infected saliva, usually through bites or scratches. This viral, neuroinvasive disease causes severe encephalitis (brain inflammation) in warm-blooded animals.The virus also enters the salivary glands in high concentrations, leading to further transmission. Once the signs and symptoms of the virus arise, there is no treatment and the disease is usually fatal. The disease is prevalent in nearly every continent of the world, with over 55,000 human deaths a year, 95% of which occur in Africa and Asia.[3]
Genome structure
Rabies is a negative, single-stranded, enveloped RNA virus. The RNA is tightly bound within a ribonucleoprotein complex. The virus' genome encodes 5 proteins: nucleoprotein (N), phosphoprotein (P), matrix protein (M), glycoprotein (G), and polymerase (L). Glycoprotein acts as a catalyst in crucial pathogenic processes, such as the virus binding to host cell receptors, as well as membrane fusion, which enables the viral genome to enter the cytoplasm of the host's cells. The genome is non-segmented, linear antisense RNA. RNA-dependent RNA transcriptase and some structural proteins are present in the nucleocapsid.
Virus structure
The virus has a cylindrical shape; one end is rounded while the other is planar or concave. The virus’s lipoprotein envelope contains about 400 spikes on its surface, which are composed of glycoprotein (G). The spikes do not cover the planar end.Within the envelope lies the membrane or matrix (M) protein layer, which may be invaginated at the planar end. The virion’s core consists of helically arranged ribonucleoprotein, which consists of protein and RNA. The Negri Body, a specialized structure within the cytoplasm which is typical for a rabies infection, is the site of viral transcription and replication.
Ecology (Hosts, Transmission, and Life Cycle)
Rabies is a zoonotic disease and is transmitted by mammals, usually as a result of an infected animal bite. A neuroinvasive disease, it causes severe encephalitis in warm-blooded animals. Multiple variants of the virus have been identified worldwide, each of which are linked to a single wild animal host, termed a “reservoir of infection” for a specific geographic region. For instance, in British Columbia, Canada, insectivorous bats (adapted to feeding on insects) are the only reservoir of rabies. However, other potential hosts exist, including terrestrial mammals, such as domestic dogs and cats, raccoons, skunks, foxes, wolves, and coyotes, though the virus is not maintained in these populations.[4] Contrary to popular belief, rodents, such as mice and squirrels, are seldom infected. Unlike many rabid mammals, bats may get sick and die before showing symptoms common to other mammals. In Africa and Asia, dogs are the main carriers of the disease and are responsible for a majority of human rabies deaths worldwide. However, in developed countries, rabies is most prevalent in wild animals. In 2003, rabies caused by exposure to wildlife accounted for more deaths than that resulting from exposure to rabies-infected dogs in South America.[5] In the U.S., the CDC reports that the majority of rabies cases occur in bats, raccoons, skunks, and foxes. In fact, currently over 90% of annual cases reported to the CDC occur in wildlife, whereas, before 1960, the majority of cases were in domestic animals. Today, domestic animals account for less than 10% of reported rabies cases. Of these animals, dogs, cats, and cattle are reported most often to be rabid.[6]
There are three known stages of rabies in animals. The first stage, the prodromal stage, lasts one to three days and marks the beginning of behavioral changes, such as loss of fear or unusual friendliness. The second, excitative stage lasts three to four days and is characterized as “furious rabies,” with symptoms including exceptional aggression and unprovoked attacks. The third, paralytic stage is caused by motor neuron damage. Here, prevalent symptoms include difficulty with coordination, paralysis, seizures, signs of choking or difficulty swallowing food or water, and frothing at the mouth. Other abnormal behaviors include depression, odd vocalizations, appearance of nocturnal animals during the day, and, in carnivores, evidence of having attacked porcupines. Death usually results from respiratory arrest.[7]
In addition to bites by infected animals, rabies can be transmitted by infected animal licks or saliva that come into contact with the mucous membranes of the eyes, nose, lips, or skin wounds. The virus is inactivated by external factors, such as exposure to direct sunlight, ultraviolet radiation, chemicals, detergents, and strong acids and bases, and thus, cannot thrive in the environment.[8] From the wound of entry, the rabies virus quickly travels along neural pathways first to the peripheral nervous system and then, via nerves, to the central nervous system (brain and spinal chord). At this point, the virus is not immediately evident within the host and vaccination may lead to cell-mediated immunity, which will prevent the symptoms of rabies in the host. Once the virus reaches the brain, it replicates and then spreads to other organs of the body via the nervous system. At this prodromal stage, symptoms appear and treatment is ineffective. The salivary glands in the mouth and cheeks receive a high concentration of the virus, thereby facilitating further viral transmission when the diseased animal bites another animal.[9]
Pathology
In humans, early symptoms of rabies are nonspecific and include fever, headache, and overall lethargy. As the disease progresses, neurological symptoms emerge, including anxiety, insomnia, confusion, violent movements, partial paralysis, agitation, hallucinations, hyper-salivation, difficulty swallowing, and hydrophobia (fear of water), which is also another name for the virus. If left untreated, rabies is always fatal in humans and death can occur within days of symptom onset.[10] In the final stages, symptoms include periods of mania and lethargy in the patient, and eventually, coma. Death may result from respiratory insufficiency, brain swelling, or pneumonia. This usually occurs two to ten days after the first symptoms, and the few humans known to have survived the disease all suffered from severe brain damage. The period between infection and the first flu-like symptoms normally occur between two and twelve weeks, but may even last up to two years. Transmission between humans is very rare though there are documented cases associated with transplant surgery.[11] Even more rarely, transmission may occur through bites, kisses, and sexual relations. Only six people are reported to have survived symptomatic rabies, while two survivors received no rabies-specific treatment either before or after the onset of illness.
Current Research
1) A change in rabies post-exposure treatment guidelines after decision analysis in Israel [12]
The Haifa District Health Office, Ministry of Health, in Israel, conducted a research study from 11/1/1999 to 12/31/2002 on physicians’ compliance with rabies post-exposure prophylaxis guidelines issued by the Public Health Services in 1997 and updated in 2003. In Israel, decisions to vaccinate are the exclusive decision of public health physicians in the district health offices, affording the process a measure of expertise. As part of the study, several variables significantly influenced physicians’ decision to vaccinate or not.
Although the incidence of rabies in Israel has declined from 97 cases in 1998 to 43 cases in 2003, rabies remains a significant public health problem in Israel, thus indicating the importance of compliance to a rabies post-exposure prophylaxis. Each year, between 16,000-20,000 people report to the district health offices after being bitten or scratched by animals; 16-18% receive rabies post-exposure treatment. Treatment guidelines emphasize four levels of risk based on the type of animal exposure. Vaccinations are required of those exposed to wild or unidentified animals, whereas vaccinations are not deemed necessary following rodent bites, or exposure to large, domestic farm animals. In the study, of 5,037 cases of animal exposure reported, 2,477 (~50%) were audited. The observed physician compliance rate was 2,437/2,477, or 0.984 (P<0.001), with a kappa coefficient of 0.803, indications of high compliance. Decisions to vaccinate were more common for those aged 15-44 and soldiers, and were 2.3 times more likely for bites versus scratches. Absence of provocation of the animal was 2.8 times more likely in those vaccinated versus those not vaccinated. Events in “rabies enzootic” geographical regions were 1.7 times more likely to result in vaccinations than those in rabies free zones. Finally, senior physicians recommended vaccination 1.2 times more than residents. Listed in descending order, the variables that influenced the decision to vaccinate were type of animal, type of exposure, and definition of area as rabies enzootic. Also statistically significant were being a soldier, provocation, and being a senior physician. Regarding type of animal, the guidelines had initially grouped all domestic animals in a single risk category, but were later revised to state explicitly that, according to the epidemiology of rabies in Israel, identification of cat rabies is relatively rare, and thus there is a much lower risk of contracting rabies following exposure to cats.
The study showed that 52% of decisions to vaccinate depended on geographic location of exposure. However, the Veterinary Services argued that Israel, being a small country with no natural borders, should be considered rabies enzootic in its entirety. On the other hand, public health physicians maintained that rabies activity has remained confined to certain areas for a long time, such as in the Judean desert and in the areas surrounding the Palestinian Authority, whereas no events have been reported in the cities of Tel Aviv and Haifa. A decision to consider all areas rabies enzootic would involve vaccinating an additional 585 people, or 3.1 times as many people, which, upon extrapolating these numbers to the entire country, would lead to an additional 5,580 people being vaccinated per year, costing the country an extra 2.6 million dollars. Thus, the guidelines have retained the classification of geographic areas as rabies enzootic or rabies free.
U.S. reports of post-exposure prophylaxis, including one made in Florida between 1997 and 1998, have shown that in ¼ of cases, people received unnecessary treatment, with the total cost of one mass treatment equaling 1.1 million dollars. Israel’s rate of unnecessary treatment has been found to be much lower than that reported in the U.S. study (1% versus 40%). Also, physician compliance rate was much higher in Israel than in the U.S. (98.4% vs. 91.5%). These results have largely been attributed to the fact that expert public health physicians in Israel are the sole decision-makers in regards to post-exposure treatment, whereas in other countries, all physicians, some of whom are not as knowledgeable about the issues at hand, are entitled to make decisions about rabies prevention.
2)Oral Rabies Vaccine (ORV) Bait Uptake by captive striped skunks[13]
Skunks are a major reservoir and vector of rabies in the United States, but unlike oral rabies vaccine programs for foxes, raccoons, and coyotes, oral vaccines for use in skunks is not licensed. Skunks have smaller jaws and exhibit different feeding behaviors than other species, so the current oral rabies vaccine (ORV) campaigns may not be applicable to skunks. Thus, a study was conducted to assess striped skunks' handling and ingestion of currently used ORV baits. The variables measured were bait selection frequency, vaccine container (VC) puncture frequency, and consumption. Results showed that bait characteristics such as flavor, texture, and size, had an affect on selection and consumption. In three of four trials, skunks showed a preference for fish and chicken flavors, and consumption was more likely if the VC was directly coated with the bait matrix. Also, improved baits would be of smaller size and contain a slightly pressurized VC to increase the possibility of VC puncture and ingestion of vaccine by the skunks.
3)Transmission of Rabies Virus from an Organ Donor to Four Transplant Recipients[14]
In May 2004, Texas physicians diagnosed four transplant recipients with encephalitis, all of whom lapsed into comas and died within 50 days after transplantation. Three of the patients were recipients of a liver and two kidneys from a common donor, while the fourth had received a vascular graft from the same donor during liver transplantation. All patients showed rapid neurologic deterioration, which manifested as agitated delirium and seizures. About 48 hours later, they experienced respiratory failure, and needed to be intubated. The patients died an average of 13 days following the onset of neurologic symptoms. The organ donor had succumbed to a subarachnoid hemmorhage, associated with hypertension, four days after having been admitted to the hospital with altered mental status and requiring intubation, as well as having gone to several emergency departments with symptoms of nausea, vomiting, and difficulty swallowing. Upon hospital admission, the patient’s urine tested positive for cocaine and marijuana, although donor-eligibility screening and testing of premortem blood, urine, and bacterial cultures showed no signs or symptoms of infection that would preclude organ donation. However, following the donor's death, the transplants, and the rabies diagnoses in the four patients, it was reported in contact investigations of the donor's friends that he had reported being bitten by a bat.
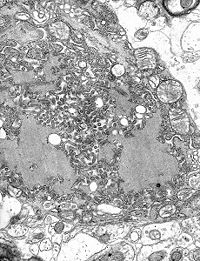
The primary mode of Rabies transmission in the U.S. is through the bite of an infected bat. Tissue and blood specimens from the four patients and donor were studied in the laboratory through various serologic analyses and fluorescence microscopy to detect viral antigens in tissues. Cytoplasmic inclusions consistent with Negri bodies were found throughout the central nervous system, particularly in cells of the cerebellum and in neurons of multiple parts of the brain, such as the frontal cortex, thalamus, hippocampus, midbrain, and pons. For instance, electron microscopy of the midbrain of one of the patients showed many rhabdovirus particles. Direct fluorescence antibody staining of other neurons throughout the CNS showed intracytoplasmic rabies virus antigens. Antibodies were found in reactive patients 35-36 days after their operations. The particular rabies virus variant found through antigenic typing was that associated with bats. In the lab, suckling mice were also inoculated intracranially and intraperitoneally with cerebrospinal fluid and 10% tissue suspensions from the patients’ brain, spinal chord, and kidneys. Of those who hadn’t died 7-8 days after inoculation, all mice were found to have neurologic abnormalities. Thin section electron microscopy of CNS tissue showed rhabdovirus particles and another test showed rabies virus antigen on staining with DFA.
This article indicates the dire need for improvement in detection and prevention of transplant-transmitted infections, such as enhanced screening of donors, diagnosis of illness in recipients, and the establishment of standardized methods of storage and use of donor vascular segments. The Organ Procurement and Transplantation Network (OPTN) has responded by creating standards that require organ-procurement organizations to determine the risks of infectious diseases through blood testing for viral pathogens in the blood and syphilis, and through various screening questions. A possible revision of these standards would widen the list of potentially transmittable diseases, because currently, laboratory testing for and questions regarding rabies are not included. Another improvement would involve better national detection of infection risks to transplant recipients by allowing connections to common donors to be made. As of now, diagnosing donors with infections after-the-fact is impeded by a scarce supply of donor tissue; only serum samples are stored at length.
The Department of Health and Human Services and the CDC are working on donor screening practices and monitoring of recipients but, in the meantime, a critical first step is for medical health professionals to notify their local tissue-procurement organizations in cases in which unexpected illnesses arise in transplant recipients.
References
- ↑ http://www.cdc.gov/rabies/virus.html
- ↑ http://www.cdc.gov/rabies/virus.html
- ↑ http://www.who.int/mediacentre/factsheets/fs099/en/
- ↑ http://www.unbc.ca/nlui/wildlife_diseases_bc/rabies.htm
- ↑ http://www.who.int/mediacentre/factsheets/fs099/en/
- ↑ http://www.medicalnewstoday.com/articles/7050.php
- ↑ http://www.unbc.ca/nlui/wildlife_diseases_bc/rabies.htm
- ↑ http://www.unbc.ca/nlui/wildlife_diseases_bc/rabies.htm
- ↑ http://www.unbc.ca/nlui/wildlife_diseases_bc/rabies.htm
- ↑ http://www.medicalnewstoday.com/articles/7050.php
- ↑ Srinivasan, A. et al. Transmission of rabies virus from an organ donor to four transplant recipients. New England Journal of Medicine 2005;352:1103-1111.
- ↑ Dubnov, J. et al. A change in rabies post-exposure treatment guidelines after decision analysis in Israel. European Journal of Public Health 2006;17(1):92-97.
- ↑ Jojola, S.M., Robinson, S.J., & VerCauteren, K.C. Oral rabies vaccine (ORV) bait uptake by captive striped skunks. Journal of Wildlife Diseases 2007;43(1):97-106.
- ↑ Srinivasan, A. et al. Transmission of rabies virus from an organ donor to four transplant recipients. New England Journal of Medicine 2005;352:1103-1111.
[1]↑ Dubnov, J. et al. A change in rabies post-exposure treatment guidelines after decision analysis in Israel. European Journal of Public Health 2006;17(1):92-97.
[2]↑ Jojola, S.M., Robinson, S.J., & VerCauteren, K.C. Oral rabies vaccine (ORV) bait uptake by captive striped skunks. Journal of Wildlife Diseases 2007;43(1):97-106.
[3]↑ Srinivasan, A. et al. Transmission of rabies virus from an organ donor to four transplant recipients. New England Journal of Medicine 2005;352:1103-1111.
[4]↑ http://www.unbc.ca/nlui/wildlife_diseases_bc/rabies.htm
[7]↑ http://www.cdc.gov/rabies/virus.html